Hearken1 English
-
California Schools’ Response to Pandemic Varies Widely
ByRicardo Cano, CalMatters
 Their schools sit just five miles apart on opposite ends of Southern California’s notoriously busy Interstate 405, but the gap between their students’ distance learning experiences so far has been vast.
Their schools sit just five miles apart on opposite ends of Southern California’s notoriously busy Interstate 405, but the gap between their students’ distance learning experiences so far has been vast.In Redondo Beach off the South Bay coast, Karen Cull’s three sons began engaging with their teachers online March 18, three school days after their district physically closed campuses to combat the spread of the COVID-19 pandemic. On Monday, Redondo Beach will begin “Phase 2” of distance learning, in which teachers and students will be expected to cover new content.
In Hawthorne, an inland working-class community, Raul Torres spends five hours a day with his second-grade daughter and fourth-grade son completing paper packets. He’s heard little from their teachers in the four weeks after schools physically closed and the district doesn’t plan to roll out its distance learning program until April 21.
“It’s been challenging because, obviously, I’m not a teacher,” Torres said.
(Image: Melina, 8, and her brother Adrian, 9, play minecraft before bed. With limited classwork provided by their district the Torres kids have plenty of time for video games when their homework is finished. Photo courtesy of Raul Torres)
Across California, school districts are each frantically tackling the same challenge — how to keep students learning remotely — with varying degrees of preparedness. Conversations with parents across the state reflect existing disparities: Wealthier districts appear more likely to weather the transition with greater ease.
While school systems like Redondo Beach have been able to transition toward online learning without skipping a beat, parents in many districts have said they’ve gone weeks before hearing much about their schools’ academic plans.
A limiting factor in schools’ transitions has been access to Internet and technology and whether schools had the finances and infrastructure to provide families these resources. Across California’s 1,000 school districts, there have been longstanding inequities in the amount of funding districts have been able to locally raise for needs like student technology.
State Superintendent of Public Instruction Tony Thurmond said this week that the state is working to secure 150,000 devices for students who don’t have one so they can do online learning. Recent hotspot and Chromebook donations from Google have helped make a dent, but not enough, Thurmond said Tuesday. He asked for //calmatters.org/education/2020/04/california-schools-parents-coronavirus-remote-learning/
This email address is being protected from spambots. You need JavaScript enabled to view it. ">public donations to secure computers for students.“We have had a digital divide in this state and in this country for many years, and It’s an embarrassment, and we must change that,” Thurmond said.
State officials have said they expect that most California districts will have formally launched distance learning programs by the end of April, though scenarios such as in California’s South Bay underscore the wide variance in how schools are shifting toward it.
About 9 in 10 students in the Hawthorne district are socioeconomically disadvantaged, according to state data, but academics have praised the district for narrowing achievement gaps for its black and Latino students. More than one-third of the district’s students are English-language learners.
Before the pandemic, Torres said his 8-year-old daughter was learning a lot, challenged by a rigorous curriculum.
“She was learning things that I never learned until I was in high school,” Torres said.
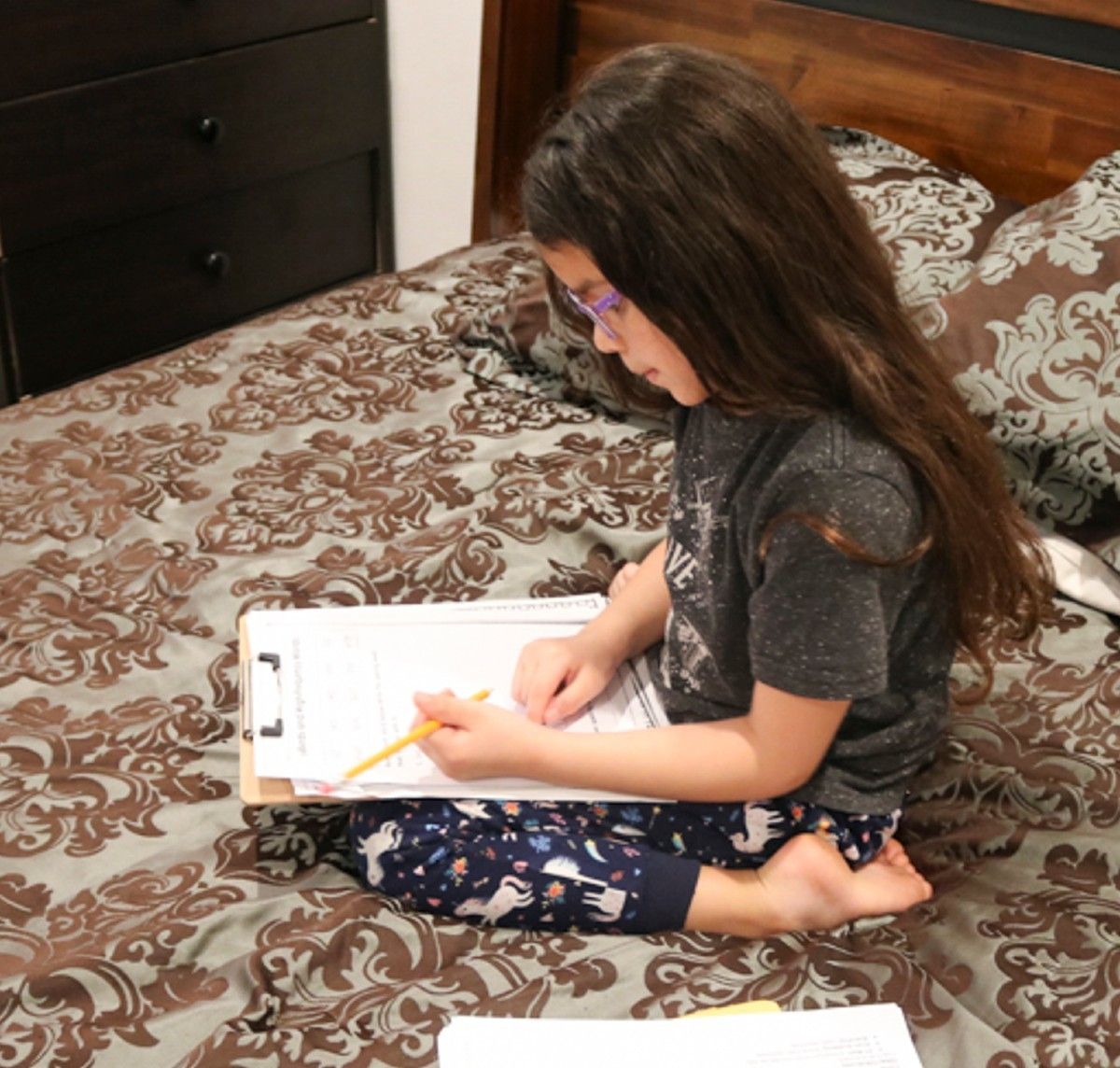 (Image: Melina, 8, does homework in her parents’ bedroom. Photo courtesy of Raul Torres)
(Image: Melina, 8, does homework in her parents’ bedroom. Photo courtesy of Raul Torres)Since his children’s schools physically closed, Torres, an electrician, has dedicated afternoons and evenings to working through two weeks’ worth of paper review packets with his kids. Torres’ autistic son has not received any special education services, he said, so he relies on the parenting classes he took to help the fourth-grader.
Torres sees the difference in distance learning as he travels to job sites across Los Angeles. Customers in Torrance and Manhattan Beach, for instance, trade notes on how far along their schools are in making the transitions.
“They already have the means to do it,” Torres said. “We don’t (in Hawthorne), not yet.”
A survey by The Education Trust-West, an advocacy group focused on closing student achievement gaps, showed widespread concerns from parents about student regression.
The poll of 1,200 California parents found that while 8 in 10 gave their schools positive marks in handling the aftermath of school closures, just 45% of respondents said that their schools were providing them with regular contact or access to their child’s teachers.
Nineteen percent of parents — including 1 in 5 Latino respondents — said they’ve received little to no academic information from their schools. Most black and Latino parents said they’re worried they don’t have the resources to keep their students from regressing.
“Long before this pandemic came, California faced an epidemic of educational inequality,” said Elisha Smith Arrillaga, executive director of The EdTrust-West, adding that school closures “will only exacerbate those gaps.”
“There is simply no way to close schools for a month without gaps in student learning,” she said. “Now is the time to accelerate planning to ensure that teachers and school leaders have the resources they need to stop those gaps in their tracks.”
In Redondo Beach, Cull praised the district’s rapid and “fantastic” response in shifting toward online. The district closed schools March 13, a Friday. By the following Wednesday, Cull’s students were taking part in online lessons covering prior materials. Special educators were quick to prepare a plan for her son with Down Syndrome, she said.
Each teacher has had different approaches to online learning, Cull said. One of her oldest son’s high school science teachers set up a class meeting using Flipgrid, where students could see each other and interact in a virtual lesson — a helpful exercise in social interaction.
“He got such a kick out of seeing the videos that the other kids have posted and just seeing other 15-year-old kids in their bedroom messing about,” she said.
About 16.5% of Redondo Beach students are socioeconomically disadvantaged, according to state data, and about 4% of students are English learners. Like Torres, Cull also trades notes with other parents. She says she and her sons are in “a very lucky place right now.”
“What this is doing is exacerbating the existing differences, the existing inequalities,” Cull said. “This situation has emphasized (inequalities) because the districts like Manhattan Beach and Redondo Beach have had existing technology structures already there.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Coronavirus Could Force Private Practices To Close Or Sell — Raising Costs
By Kristen Hwang for CalMatters
 In a matter of weeks, Dr. William Goral, a private practice ear, nose and throat specialist in San Bernardino County, will be out of business.
In a matter of weeks, Dr. William Goral, a private practice ear, nose and throat specialist in San Bernardino County, will be out of business.His small, solo clinic, which has served patients throughout the Inland Empire for 30 years, postponed about 80% of patient visits due to coronavirus restrictions. That’s not enough revenue to pay rent, utilities or staff.
“We are going into the red even having laid off two-thirds of my employees,” Goral said.
At private practices and small clinics across the state, independent physicians are worried their businesses won’t survive the current crisis, forcing them to either close their doors or sell their practices, which could lead to higher patient costs. In either case, experts worry that will leave the health care system vastly diminished at a time when the state is facing skyrocketing costs and a shortage of doctors.
(Image: Dr. George Scott in one of several examination rooms in his Manteca clinic. Scott’s private OB/GYN practice is moving to a smaller clinic space in the midst of the coronavirus pandemic due to a rent increase. Photo by Anne Wernikoff for CalMatters)
About one in three Californians get care from private practice physicians and specialists, according to the California Medical Association, which represents roughly 50,000 doctors across the state. In a recent survey, nearly 76% of members reported being extremely worried or very worried about finances.
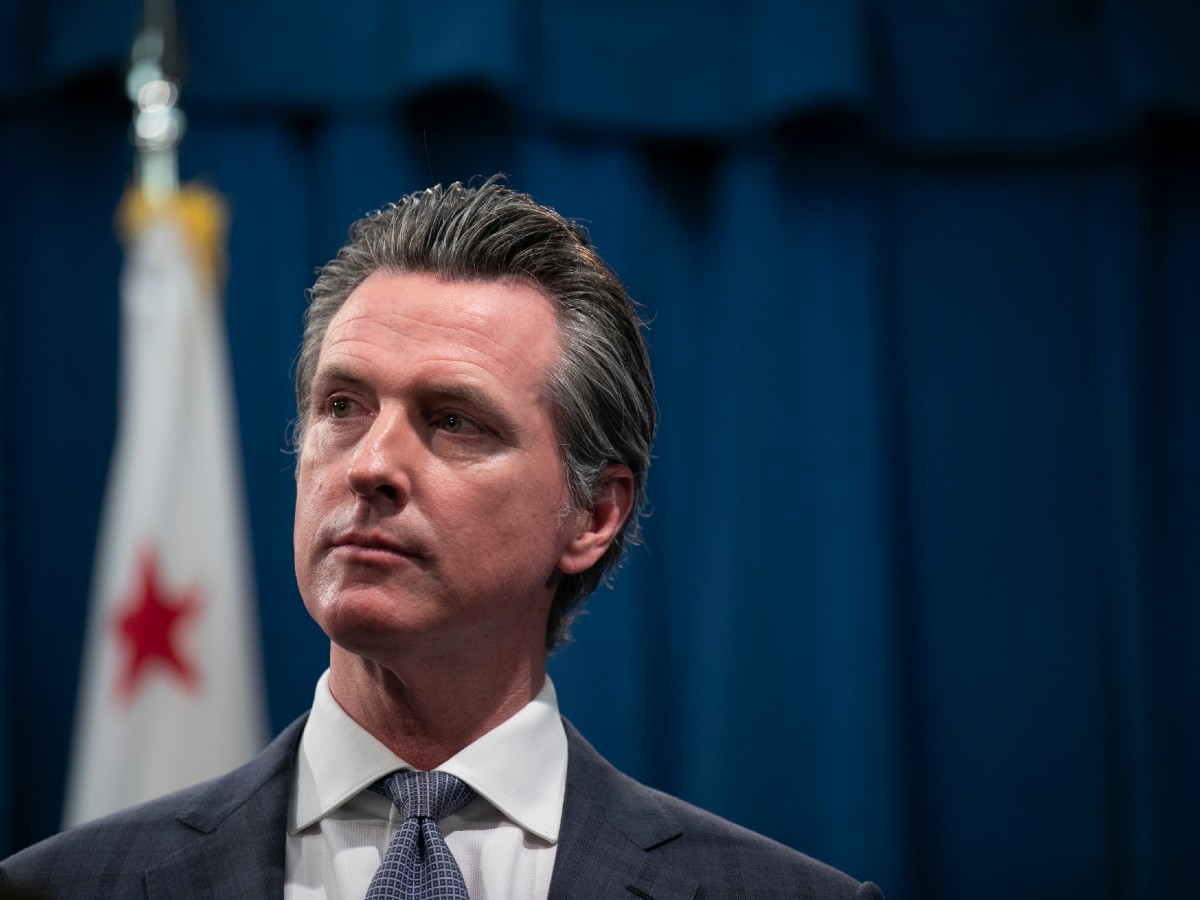
Empty clinics triggered a cash crunch for doctors after Gov. Gavin Newsom issued a shelter-in-place order last month. That’s because the statewide lockdown forced a majority of medical procedures, from hip replacements to annual check ups, to be canceled or delayed unless they are deemed an emergency.
A catastrophe for private practices
On Wednesday, the governor announced plans to resume some delayed medical care such as heart valve replacements, angioplasty and and tumor removals, but he warned the state remains far from reopening.
And though the federal government is providing aid, most say it’s not nearly enough.
“The whole situation is catastrophic for the entire profession in terms of economics,” said Dr. Thomas LaGrelius, a family medicine doctor in Torrance, Calif. and president of the American College of Private Physicians.
LaGrelius currently is only able to conduct about three in-person patient consults per day and has tried to switch as many appointments as possible to online video conferences. Unlike other doctors who received emergency grants this week from the U.S. Department of Health and Human Services, LaGrelius’ clinic has yet to get any relief from the federal Coronavirus Aid, Relief and Economic Security Act, or CARES Act.
The federal department, which is doling out $100 billion to doctors based on the amount of patients they serve who are on Medicare, gave him a test deposit of $0 and told him a grant would come later.
And while grants are certainly welcome, they’re a “drop in the bucket,” said Debbie Rood, business manager for her husband’s obstetrics and gynecology practice in Manteca. Rood’s husband Dr. George Scott said they received about $2,000 since most women over the age of 65 don’t see a gynecologist regularly.
His private practice’s finances are complicated by the fact that insurance companies won’t reimburse him until after patients give birth, leaving him and his staff performing unpaid labor for months. At the same time, their rent tripled, forcing them to downsize to a smaller clinic.
Taking out a second mortgage
Scott and Rood are determined to keep the business running but they may need to take a second mortgage on their home. They are also concerned about the long-term implications the economic crisis will have on access to care.
“If you lose all of your primary care doctors and your (obstetricians) because you can’t make a living,” Rood said, “where are patients going to go?”
It’s a question with a complicated answer, said James Robinson, professor of health economics at UC Berkeley. The economic fallout of the pandemic will lead to the closure of many private practices, but the implications are less clear.

Consolidating practices
Increasingly, in the past decade, independent doctors and private community hospitals have been swallowed by sprawling health care delivery systems through mergers and buyouts. Nearly 60% of Californians received care from an integrated healthcare system in 2018, which organizes doctors, hospitals, and sometimes insurance companies into one coordinated system, according to Let’s Get Healthy California, a state task force that monitors key health indicators including access to care.
Because small businesses like independent physicians typically don’t have the financial reserves to ride out severe economic downturns, the current pandemic will hasten the consolidation of healthcare, Robinson said.
“I think that it’s going to drive them into the arms of health plan places like Kaiser,” Robinson said.
The loss of private practices isn’t necessarily a bad thing, experts say. Consolidated health care can lead to better communication between doctors, more efficient use of testing and scans, and more cost-effective treatment, he added.
(Image: Debbie Rood and Dr. George Scott in their Manteca clinic. Rood says making sure Scott stays healthy during the coronavirus pandemic is a priority. Photo by Anne Wernikoff for CalMatters)
The problem is many of California’s rural counties, which often face provider shortages to begin with, still rely on private physicians and community health clinics. Forty of the state’s 58 counties had below-average access to consolidated health care in 2018, with as little as 10% of the population in Del Norte enrolled in a managed health care plan.
Mergers raise costs on patients
A large body of evidence shows that hospital mergers and physician buyouts have increased insurance prices throughout the state.
In areas with high hospital consolidation and high proportions of hospital-owned physician practices, health insurance premiums cost up to 12% more than in areas with average levels of consolidation, according to research published in Health Affairs, a peer-reviewed health policy journal.
“There was an uptick in merger activity right after 2008,” said Daniel Arnold, co-author of the paper and research director at the Nicholas C. Petris Center on Health Care Markets and Consumer Welfare at UC Berkeley. “I think you will see something similar here.”
Rood said she’s scared to death of what will happen to patients should her husband, Scott, become ill from coronavirus or should their private practice be forced out of business. Already, with only five obstetricians and gynecologists in their area and one planning to leave in June, Scott said there aren’t enough OB-GYNs to take emergency calls at the local hospital.
Like many other doctors and business owners, Rood and Scott applied to the Small Business Administration’s Paycheck Protection Program, a $350 billion emergency fund created by Congress to avert business closures and layoffs during the COVID-19 pandemic.
Last hope hangs on second relief package
Their bank, however, took 11 days to send the application to the first-come, first-serve relief program. The day after they submitted, the Small Business Administration announced it had run out of money.
Now, with Congress approving a second $484-billion relief package with $75 billion set aside for physicians and hospitals, independent physicians like Scott and Goral are hoping to save their life’s work.
Goral, the ear, nose and throat specialist, was unsuccessful in obtaining help in the first round of federal funding, but he hopes the second round of funding will buy time until patients return. Still, his position is precarious. Each passing day pushes his business further into debt and he fears he’ll close before ever seeing any money.
“If we have to shut our doors and we don’t have a practice anymore, then the opportunity has been missed,” Goral said.
Kristen Hwang is a freelance reporter pursuing joint master’s degrees in public health and journalism at UC Berkeley.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Coronavirus Detectives: Here’s How Counties Try to Track Everyone Exposed
ByRachel Becker, CalMatters
 By the time public health officer Bela Matyas learned that the novel coronavirus was spreading in Solano County, the patient in her 40s was already on a ventilator.
By the time public health officer Bela Matyas learned that the novel coronavirus was spreading in Solano County, the patient in her 40s was already on a ventilator.Back in February, the woman was the first in the nation known to be infected without traveling or being around someone who was sick. But she was too ill to answer questions about where she’d been and whom she had talked to, worked with and touched.
Dozens of public health investigators from local, state and federal agencies fanned out like detectives, questioning the family members who had visited her and the hospitals that had orchestrated her care — even staking out the store where she worked. Their mission: to piece together a list of people who could have been exposed to the virus.
In the end, the list totaled more than 300 people spanning six California counties, Matyas estimated. Four — including three healthcare workers — tested positive, each prompting their own investigation.
(Image: U.S. Air Force photo by Airman 1st Class Taylor D. Slater)
This process, called contact tracing, is a critical element in containing the spread of the novel coronavirus. But the ability of California’s 61 county and city public health departments varies greatly as they struggle to keep pace with rising numbers of patients.
“What we had to do was clear from the beginning,” Matyas said. “But actually being able to do it was very hard.”
Some local health departments, like Madera County’s, have managed to trace the contacts of every person who tests positive for the coronavirus. Others, like the city of Long Beach and Placer County, are so overburdened that they are only trying to trace contacts that could put vulnerable people at risk, such as healthcare workers or people in nursing homes.
To handle the pandemic, the nation will need 30 contact tracers for every 100,000 Americans, according to the National Association of County and City Health Officials. But no California city or county has anywhere near that many. Under that formula, for example, Long Beach would need 140 investigators, seven to nine times more than it has now.
North of Sacramento, Placer County, with a population of almost 400,000, would need 120 tracers.
“It certainly illustrates the point that 18 — which is our expanded capacity, which is more than our baseline of six — is woefully inadequate,” said Aimee Sisson, Placer County’s public health director.
Contact tracing will become even more important as the state starts reopening parts of its economy. The concern is that more human interaction could cause flare-ups, especially since people can spread the virus before feeling ill and limited testing leaves people unaware they’re infectious.
“We need to make sure that there is capacity in every county to do adequate contact tracing. That’s part of containing the disease,” said Kat DeBurgh, executive director of the Health Officers Association of California. “Are we ready today? No. When will we be ready? I don’t know.”
Gov. Gavin Newsom addressed the concern about inadequate contact tracing on Wednesday, announcing plans to train 10,000 people to help local health departments. “The good news is we believe we have the capacity to build an army of tracers,” Newsom said, although he did not say when they’d be ready to deploy.
Jeffrey Martin, a professor of epidemiology and biostatistics at the University of California, San Francisco, said that fighting an epidemic is like fighting a wildfire: The state can’t afford to mess up containment.
“[It’s] important to track all of those people down to extinguish all the embers in that brushfire,” Martin said. “If we don’t do it right, and if the brush fires are not extinguished, you’d have to be a magical, wishful thinker, to think that there would not be a raging wildfire.”
Some counties keep up, others can’t
The San Joaquin Valley county of Madera typically has two to three people keeping tabs on tuberculosis and sexually transmitted infections in its population of roughly 157,000 people.
Then, the coronavirus hit — and the initial cluster encompassed about 200 patients and potential contacts, said Madera County public health director Sara Bosse. Thirty-six people have tested positive.
Still, by teaming with the sheriff’s department and probation investigators, the county has managed to keep up contact tracing, isolation and quarantine for everyone potentially exposed.
Madera is unusual in that investigators, typically in plain clothes, visit patients and their contacts in person — sort of. They drop off packets of information as well as a letter excusing work absences to employers. Then they get back into their cars, and answer questions face-to-face through the window, over the phone.
“Then they can explain to them what’s going on,” Bosse said. “We understand that people are experiencing a lot of anxiety and it’s difficult for people to hear this news that they might have been exposed.”
For now, the spread of the virus seems to be slowing. “We’re really hopeful that it’s at least in part due to the active contact tracing that we’ve implemented,” Bosse said.
In Riverside County, cases are coming in faster than the county’s 30-plus person team can investigate them, according to Barbara Cole, branch chief of disease control for the county’s public health department. The county has 3,084 confirmed cases.
It can take multiple phone calls to build enough trust to reconstruct someone’s string of contacts, Cole said.
“It’s about trying to establish a rapport, stressing how we’re going to protect their confidentiality,” she said. “The majority of people, they’re concerned about their friends and their family.”
In the Northern California county of Solano, Matyas quickly realized that tracing and quarantining all contacts would be impossible for every case. To date, 186 people have tested positive in the county.
Instead, the county focuses on tracking the risk to vulnerable populations, including people who are older, have underlying medical conditions, or live without shelter.
Solano County’s communicable disease team, which has shrunk to its original staff of six, first interviews anyone who tests positive about where they work and who they came in contact with. That in some cases is a long list: people who visit their homes, coworkers who sit close or share food.
Then a member of the team calls all of the contacts. The idea is to identify and isolate people who are feeling ill or whose jobs put them at risk of infecting others in nursing homes, hospitals, or homeless shelters.
“We no longer pretend that we can do any kind of active quarantine,” Matyas said. “There’s no bandwidth to check on them to see if they’re doing it.”
Long Beach and Sacramento and Placer counties also are only tracing the virus’s spread through vulnerable populations.
“Instead of asking every place you went to, every person you came into contact with, we say, ‘Have you been in contact with vulnerable populations?’” said Sisson in Placer County. “We just have too many cases for that full interview.” In the county, which is home to the first person to die of the novel coronavirus in California, 133 people have tested positive.
In Long Beach, every case initially was tracked. But then people kept getting sick, and most of the deaths are in long-term care facilities
As people sheltered in place, contact tracing didn’t have to be as extensive. “Now we’re to the point where we have more than 400 cases, and we’re really focusing on our healthcare worker cases, and our cases in our long-term care facilities,” said Emily Holman, communicable disease controller for the city’s health department.
Tracing contacts of people in long-term care facilities is different than in the community at large. Instead of focusing on reconstructing a web of contacts, the aim is to rapidly identify and separate infected and potentially exposed people from healthy people. Speed is key, so if someone’s symptomatic, they’re treated as a case even with no test results.
“Every minute in those facilities can be crucial and could prevent an exposure,” Holman said.
Staffing up
Former CDC Director Tom Frieden called for an army of more than 300,000 contact tracers in an interview with STAT. And current CDC head Robert Redfield announced plans to hire 650 more public health personnel, including to help with contact tracing, the Washington Post reported.
Local health departments have been bolstering their workforces on their own. San Francisco plans to recruit and train as many as 150 people to conduct contact tracing, including librarians, city attorney staff and medical students.
The Bay Area’s Alameda County also has ramped up from just seven staff investigating cases of communicable disease to 60 people assigned to the novel coronavirus — including 18 who follow up with contacts. As the epidemic progresses, “we anticipate deploying as many as 300 staff for contact tracing,” said Nicholas Moss, acting director of Alameda County’s Public Health Department.
Sacramento County is working to expand its six-person team to 30 by recruiting from other departments and training medical students to work with people who are homeless.
“We’re hoping that based on the modeling that’s occurring, that we will be ready — and actually, we’re hoping that there won’t be another wave,” said Public Health Officer Olivia Kasirye.
Is there an app for that?
Some counties are looking to technological help. San Francisco, for instance, is training its contact tracers to use a platform that Grant Colfax, director of public health, called “an integral part of our efforts going forward.”
The platform, developed by a software company called Dimagi, is not an app that people can download to their phones. Instead, it’s a web portal that public health workers can use to keep tabs on people with infections, list their contacts and keep in touch.
Apple and Google also have proposed tracking people’s proximities using Bluetooth. Newsom has said the state is vetting various technologies.
But Alameda County’s Moss is cautious about protecting the privacy of residents.
“We want to make sure that any technological tool we employ where people’s health information is going to be input, that there are adequate safeguards for privacy,” Moss said. Plus, the app has to be easy to use, and it has to cough back up the data needed to keep tabs on the virus’s spread.
Eric Sergienko, Mariposa County’s health officer, worries that if each local health department ends up using different software, it might be hard to trace contacts that cross county lines.
That’s where Sergienko hopes the state steps in and standardizes the platform California’s counties use. “What can the state do for us? Just by finding the best one,” he said.
State Health and Human Services Secretary Mark Ghaly said that California will need 10,000 more contact tracers as it modifies its stay at home order. Between 2,000 and 3,000 people could test positive per day. And each of them could have ten contacts, he said.
California might not have needed to push quite so hard to ramp up during the crisis if it had funded enough public health workers to begin with. “We’ve been seeking increased funding for years,” said Kat DeBurgh, executive director of the Health Officers Association of California.
More trained health workers could be important in fending off the next pandemic.
“By having these trained contact tracing public health workers, we can actually prevent infections, prevent the severe disease from happening in the first place,” said Lee Riley, a professor of epidemiology and infectious diseases at the University of California, Berkeley’s School of Public Health.
“But right now, everything that we’ve been doing is just reactive to what’s already happened.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
COVID Bailout Cash Goes to Big Players That Have Paid Millions to Settle Allegations of Wrongdoing
By Rachana Pradhan and Fred Schulte, Kaiser Health News The Trump administration has sent hundreds of millions of dollars in pandemic-related bailouts to health care providers with checkered histories, including a Florida-based cancer center that agreed to pay a $100 million criminal penalty as part of a federal antitrust investigation.
The Trump administration has sent hundreds of millions of dollars in pandemic-related bailouts to health care providers with checkered histories, including a Florida-based cancer center that agreed to pay a $100 million criminal penalty as part of a federal antitrust investigation.At least half of the top 10 recipients, part of a group that received $20 billion in emergency funding from the Department of Health and Human Services, have paid millions in recent years either in criminal penalties or to settle allegations related to improper billing and other practices, a Kaiser Health News review of government records shows.
They include Florida Cancer Specialists & Research Institute, one of the nation’s largest U.S. oncology practices, which in late April said it would pay a $100 million penalty for engaging in a nearly two-decade-long antitrust scheme to suppress competition. A top Justice Department lawyer described the plot as “limiting treatment options available to cancer patients in order to line their pockets.” The company, which is required to pay the first $40 million in penalties by June 1, received more than $67 million in HHS bailout funds.
HHS distributed emergency funding to hospitals and other providers to help offset revenue losses or expenses related to COVID-19. In April, it distributed the first $50 billion based on providers’ net patient revenue, a calculation that gives more money to bigger systems or institutions charging higher prices.
Companies that have attested to receiving payments as of May 4 collectively received roughly $20 billion. The list is likely to change in the coming days as other companies confirm they’ve received money.
In total, the CARES Act, signed into law by President Donald Trump in March, provides $100 billion in emergency funding. Subsequent coronavirus relief legislation added another $75 billion. Money has also been steered to hot spots with high numbers of COVID-19 patients, rural health care providers and the Indian Health Service.
Of the companies documented to date, other top recipients ― including Dignity Health in Phoenix, the Cleveland Clinic, Houston’s Memorial Hermann Health System and Massachusetts General Hospital in Boston — have paid millions in recent years to resolve allegations related to improper billing in federal health programs, false claims to increase their payments or lax oversight that enabled employees to steal prescription painkillers.
Dignity Health, one of the largest hospital systems in the West, received $180.3 million in HHS bailout funds, making it the top recipient listed. It has settled civil accusations by DOJ that it submitted false claims to Medicare and TriCare, the military health care program.
The Cleveland Clinic, which in 2015 paid $1.74 million to settle federal allegations that it mischarged Medicare for costly spinal procedures to increase their billings and has entered into other similar settlements, received $103.3 million from HHS, the second-largest amount.
Memorial Hermann Health System and Massachusetts General Hospital received more than $93 million and $58 million, respectively. In 2018, Memorial Hermann paid nearly $2 million to the government to settle allegations that it improperly billed government health care programs by charging for higher-cost services when patients only needed lower-cost outpatient services.
Massachusetts General Hospital in 2015 paid the federal government $2.3 million to settle allegations that lax oversight enabled hospital employees to steal thousands of prescription medications, mostly addictive painkillers, for personal use.
Malcolm Sparrow, a professor at the Harvard John F. Kennedy School of Government, said the HHS methodology for its general distribution of relief funds is “a little bit worrying.”
“If you peg the amount based on historical volume and you’ve got good reason to believe that historical volume is inflated due to fraud and abuse, the irony is that they get more money because they’re more dishonest,” Sparrow said. “But you can’t prove that in a short period of time.”
Public tolerance for fraud and abuse naturally rises during times of emergency, Sparrow said, and now is not the time to revisit historical decisions to determine which companies are entitled to federal relief based on legal issues.
“I think that’s a tough case to make,” he said.
HHS has criteria for disqualifying providers from receiving bailout money. But even the strongest condition carries a broad caveat: None of the funds may be used for grants to any corporation convicted of a felony criminal violation within the preceding two years ― unless officials have decided that it is not necessary to prohibit them from doing business with the federal government.
“It’s sort of a high bar” for someone to be disqualified for this money, said Roger Cohen, a health care lawyer at Goodwin who specializes in fraud and anti-kickback law.
The Florida oncology provider has been charged with a felony and admitted to an antitrust crime, however federal prosecutors agreed to defer any prosecution and trial because a criminal conviction would have “significant collateral consequences” for its patients, the DOJ said.
Beyond that, HHS in its terms states that providers have to certify that they are not excluded from participating in federal health care programs like Medicare and Medicaid and have not had their Medicare billing privileges revoked.
The HHS Inspector General has the authority to exclude practitioners and health care companies for a wide variety of reasons — including a conviction of fraud ― but it’s highly unusual for the federal government to do so with large institutions, experts say.
“I imagine there would be hesitancy to exclude the provider,” Cohen said. “I think you’d have concerns about interrupting access to care.”
An HHS spokesperson declined to comment on its existing allocations but said the department has rules in place to recoup funds and address fraudulent activity if necessary.
“Failure to comply with any term or condition is grounds for HHS to recoup some or all of the payment from the provider,” the spokesperson said.
In a statement, Florida Cancer Specialists signaled it intended to use the funding.
“During this health crisis, we have continued to keep the doors of our more than 80 facilities open to ensure that cancer patients have access to care and treatment,” Thomas Clark, the company’s chief legal officer, wrote in an email. “We plan to use these funds, if needed, in accordance with government guidelines to continue providing affordable, safe and high-quality cancer care.”
Dignity Health said, “We have had to bear significant costs to prepare for and manage the pandemic in our communities even as patient volumes have been dramatically reduced across our hospitals.”
In October 2014, Dignity agreed to pay $37 million after the Department of Justice alleged it admitted patients to 13 of its hospitals in California, Nevada and Arizona who could have been treated on a “less costly, outpatient basis.” The civil case involved patients treated for elective heart procedures, such as pacemakers and stents, and other conditions. The company did not acknowledge wrongdoing in settling the case.
“Charging the government for higher-cost inpatient services that patients do not need wastes the country’s vital health care dollars,” acting Assistant Attorney General Joyce Branda for the Justice Department’s Civil Division said at the time. “This department will continue its work to stop abuses of the nation’s health care resources and to ensure patients receive the most appropriate care.”
Dignity said that independent annual audits were conducted after the False Claims Act settlement in 2014 and “no additional concerns were raised related to this issue.”
Massachusetts General Hospital and Memorial Hermann did not respond to requests for comment. The Cleveland Clinic confirmed the amount of money received from HHS but declined to comment further.
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
-
COVID-19: Food Resources
 Food is top of mind for many during the COVID-19 pandemic — how to keep your family fed amid layoffs, concerns about grocery outings and food transmission, all while trying to maintain social distance.
Food is top of mind for many during the COVID-19 pandemic — how to keep your family fed amid layoffs, concerns about grocery outings and food transmission, all while trying to maintain social distance.If you’re struggling to put food on the table, have questions about food safety or need help safely getting groceries, here are some resources to help.
(Image: Pexels / Vicki Moore)
Looking for these resources in Spanish? Click here.
Help getting food
SoCoEmergency.org: Sonoma County says food assistance is available, but because of the increased demand on local organizations, your first resource should be family, friends, neighbors and/or caregivers who can assist you.
If you still need help, visit their food assistance web page to learn more about local services for able-bodied individuals, seniors, children and more.
Redwood Empire Food Bank: The Redwood Empire food bank is operating. See their website for information on how they are responding to the pandemic, including where to get food.
Catholic Charities: Catholic Charities is providing food distribution and other resources. See a map of where to get food here.
CalFresh: Monthly food benefits are available for low-income individuals and families. Find information about how to apply here. The Sonoma County Human Services Department can also help connect you to these public benefits.
211Sonoma Search for Food Pantries: Search for food pantries near you in Sonoma County.
SF Chronicle Searchable Database for Grocery Delivery: Search through a directory to help you order produce, meat and pantry goods during shelter in place.
SF Chronicle Searchable Database of Restaurants Delivering:Find Bay Area restaurants that are offering delivery during the pandemic.
Food Safety
Consumer Reports: How to Protect Yourself While Shopping
FDA: Food Safety and the Coronavirus
NPR: No, You Don’t Need To Disinfect Your Groceries. But Here’s How To Shop Safely
NPR: How Safe Is It To Eat Takeout?
Local Stores
A list of Sonoma County grocery stores offering delivery, pick-up or senior hours can be found on the county website.
Oliver's: Actions We're Taking on Coronavirus
Safeway: Answers to Your Covid-19 Questions
Helping Others with Food and Donations
Press Democrat: Here are some suggestions from the Press Democrat on how to help others during the pandemic.
Volunteering: Find local volunteer opportunities from the Center for Volunteer and Nonprofit Leadership.
-
COVID-19: Leaders Discuss Food Insecurity and Safety
 During our Coronavirus Virtual Town Hall on April 14, we invited leaders from around Sonoma County to discuss how they are keeping our community fed. Some families are lacking the daily lunches and other meals provided by schools; many have lost jobs or the work that put food on their tables; others with the means to go shopping worry about whether the food and packaging in grocery stores is safe.And the workers who pick, pack, ship, shelve, cook and serve the food are essential, of course, but put themselves at risk every day.On our panel: Juan Torres is Asst. Director, Community Connections with Catholic Charities of Santa Rosa; David Goodman is CEO of Redwood Empire Food Bank; and Eric Meuse is General Manager of Oliver's Markets.Here's a link to some of the food and nutrition resources mentioned in the video, and others.
During our Coronavirus Virtual Town Hall on April 14, we invited leaders from around Sonoma County to discuss how they are keeping our community fed. Some families are lacking the daily lunches and other meals provided by schools; many have lost jobs or the work that put food on their tables; others with the means to go shopping worry about whether the food and packaging in grocery stores is safe.And the workers who pick, pack, ship, shelve, cook and serve the food are essential, of course, but put themselves at risk every day.On our panel: Juan Torres is Asst. Director, Community Connections with Catholic Charities of Santa Rosa; David Goodman is CEO of Redwood Empire Food Bank; and Eric Meuse is General Manager of Oliver's Markets.Here's a link to some of the food and nutrition resources mentioned in the video, and others. -
COVID-19: Santa Clara County Resources
 Santa Clara County’s Public Health Department is providing detailed information about COVID-19 cases, deaths and hospital capacity on several data dashboards available online.
Santa Clara County’s Public Health Department is providing detailed information about COVID-19 cases, deaths and hospital capacity on several data dashboards available online. The county has also assembled a variety of COVID-19 resources, as listed below and found at sccphd.org/coronavirus.
Food Distribution Map
The City of San José has launched a food distribution map (bit.ly/SCCFoodMap) with important information on countywide food distribution sites to ensure food security for those in need. In collaboration with the County of Santa Clara, non-profit community partners, school districts and faith-based organizations, the Silicon Valley Strong coalition now has 129 food distribution sites operating Monday through Friday. Visit siliconvalleystrong.org for more information on how to access food resources or to donate. Also, call 2-1-1, a 24-hour multi-lingual service, or text your zip code to 89821.
CARES Act Economic Impact Payments
The Treasury Department and the Internal Revenue Service announced that distribution of economic impact payments will begin in the next three weeks and will be distributed automatically, with no action required for most people. However, some taxpayers who typically do not file returns will need to submit a simple tax return to receive the economic impact payment. More information can be found here.
Eligible taxpayers who filed tax returns for either 2019 or 2018 will automatically receive an economic impact payment of up to $1,200 for individuals or $2,400 for married couples and up to $500 for each qualifying child.
Tax filers with adjusted gross income up to $75,000 for individuals and up to $150,000 for married couples filing joint returns will receive the full payment. For filers with income above those amounts, the payment amount is reduced by $5 for each $100 above the $75,000/$150,000 thresholds. Single filers with income exceeding $99,000 and $198,000 for joint filers with no children are not eligible. Social Security recipients who are otherwise not required to file a tax return are also eligible and will not be required to file a return.
In the coming weeks, Treasury plans to develop a web-based portal for individuals to provide their banking information to the IRS online, so that individuals can receive payments immediately as opposed to checks in the mail.
New Aid for Small Businesses
California Small Business Relief Payment Plans: Effective April 2, 2020, small business taxpayers, those with less than $5 million in taxable annual sales, can take advantage of a 12-month, interest-free, payment plan for up to $50,000 of sales and use tax liability. Payment plan requests can be made through an online portal coming soon.
Paycheck Protection Program: Small businesses with 500 or fewer employees—including nonprofits, self-employed individuals, sole proprietorships, and independent contractors—can secure funds to pay up to 8 weeks of payroll costs including benefits. Funds can also be used to pay interest on mortgages, rent, and utilities. Funds are provided in the form of loans that will be fully forgiven when used for payroll costs, interest on mortgages, rent, and utilities. Small businesses and sole proprietorships can apply starting April 3. Independent contractors and self-employed individuals can apply starting April 10. Businesses are encouraged to apply as quickly as possible because there is a funding cap.
Employee Retention Credit: The Treasury Department and the Internal Revenue Service have launched the Employee Retention Credit, designed to encourage businesses to keep employees on their payroll. The refundable tax credit is 50% of up to $10,000 in wages paid by an eligible employer whose business has been financially impacted by COVID-19. The credit is available to all employers regardless of size, including tax-exempt organizations, except for government entities and small businesses who take small business loans. Qualifying employers must fall into one of two categories: 1) business is fully or partially suspended by government order due to COVID-19 during the calendar quarter, or 2) gross receipts are below 50% of the comparable quarter in 2019. The amount of the credit is 50% of qualifying wages paid up to $10,000 in total.
Open for Business Hub: A listing of technology companies that are helping small businesses by enabling remote work throughout this period.
New Guidance for Temporary Federal Sick Leave
The Treasury Department and the Internal Revenue Service have released new guidance for the Families First Coronavirus Response Act (FFCRA) which provides small and midsize employers refundable tax credits that reimburse them, dollar-for-dollar, for the cost of providing paid sick and family leave to their employees for leave related to COVID-19.
Employees experiencing symptoms of COVID-19 who are seeking a medical diagnosis or are being advised by a health care provider to self-quarantine are entitled to paid sick leave for up to two weeks (up to 80 hours) at the employee’s regular rate of pay, or, if higher, the Federal minimum wage or any applicable State or local minimum wage, up to $511 per day and $5,110 in the aggregate.
Employees caring for children whose school have closed are entitled to paid sick leave for up to two weeks (up to 80 hours) at 2/3 the employee’s regular rate of pay or, if higher, the Federal minimum wage or any applicable State or local minimum wage, up to $200 per day and $2,000 in the aggregate.
More information can be found in this FAQ. U.S. Department of Labor Wage and Hour Division will post a recorded webinar on Friday, April 3, 2020, to provide interested parties a more in-depth description and help them learn more about the FFCRA.
Hate Crimes PSA
An unfortunate side effect to community tensions around COVID-19 is a rise in hate crimes. Santa Clara County District Attorney Jeff Rosen has released a PSA condemning these acts of violence and encouraging victims and witnesses to contact their local law enforcement agencies to report them. There are translations in Chinese, Spanish, and Vietnamese.
Guidance on New Construction Rules
Among the changes in the updated Public Health Order this week were rules further restricting construction activity. In general, most construction must cease through May 3. There are some exceptions for homeless shelters and residential housing containing at least 10% income-restricted units. There are also exceptions for essential healthcare and public works projects.
The Public Health Department has created a specific section in its FAQs for construction. The City of San Jose also created its own Construction Guidance webpage that may be helpful for many who have questions related to this issue.
FAQs about the Local Health Officer Shelter in Place Order
The county makes regular updates to the FAQ documents for the local Public Health Order as new information becomes available. These materials can be accessed in the following languages:
Shelter in Place FAQ-Vietnamese
More information and regular updates can be found on the County Public Health website and the CDC website.
If you as a labor, business, faith, nonprofit, or community leader have questions or requests for information, please contact:
This email address is being protected from spambots. You need JavaScript enabled to view it. .Any school-related questions should be sent to
This email address is being protected from spambots. You need JavaScript enabled to view it. .Elected or public officials with questions should contact:
This email address is being protected from spambots. You need JavaScript enabled to view it. . -
COVID-Plagued California Nursing Homes Often Had Problems in Past
By Jordan Rau, Kaiser Health News and Anna Almendrala When Jorge Newbery finally got through to his 95-year-old mother, Jennifer, on a video call April 18, she could barely talk or move and her eyes couldn’t focus.
When Jorge Newbery finally got through to his 95-year-old mother, Jennifer, on a video call April 18, she could barely talk or move and her eyes couldn’t focus.It was the first time he had seen her since California nursing homes shut their doors to visitors a month earlier. Immediately after the video chat, Newbery called the front desk in a panic.
“I said, ‘You gotta get her out, you gotta call 911,’” he recalled. “She’s looking like she’s about to die.”
Newbery’s mother was living at the Rehabilitation Center of Santa Monica, one of 198 nursing homes in California where at least one patient had contracted the coronavirus as of April 28, public health records show. The outbreak at the Rehabilitation Center has been worse than most, with 12 employees and 24 patients infected, including nine fatalities, according to the Los Angeles County health department.
(Image: Sgt. Nicholas Shepherd, a practical nursing specialist, and Maj. Rahul Vedprakash, assigned to Urban Augmentation Medical Task Force 352-2, walk down a hallway to the next patient at the Royal Suites Healthcare & Rehabilitation Center in Galloway Township, N.J., May 5, 2020. U.S. Army photo by Spc. Miguel Pena)
The Rehabilitation Center shares several other worrisome characteristics with many other homes beset by coronavirus infections: Historically, it has had lower-than-average staffing levels and a record of not always following basic staffing and infection control rules, a Kaiser Health News analysis shows.
Compared with homes reporting no patient infections, California facilities with one or more patients with a COVID-19 case had on average a 25% fewer registered nurses per resident in the final three months of 2019, the last period for which the federal government has published data.
In addition, 91% of nursing homes reporting at least one case of the virus had a previous health violation for not following infection control rules, while 81% of homes without reported cases had such violations. Typical violations included nurses or aides not washing their hands or wearing protective clothing around potentially contagious patients.
“With low RN staffing, it is not surprising that these facilities have had previous violations for infection control and poorer overall quality as measured by having more deficiencies,” said Charlene Harrington, a professor emerita of the School of Nursing at the University of California-San Francisco. “It is a classic situation that reaffirms what researchers have found previously, only the situation with the COVID-19 virus is far more serious than anything the nursing homes have experienced before.”
In an email, Jeffrey Huang, the administrator of the Rehabilitation Center of Santa Monica, said “we respectfully and strongly disagree” that Medicare assessments of the home’s quality predict or reflect the nursing home’s efforts to protect residents from the coronavirus. The staff was “continuing to do everything possible for keeping our residents and staff safe in these uncertain times,” Huang wrote. He declined to discuss Newbery, citing patient confidentiality.
Nursing homes have emerged as one of the places the coronavirus spreads most aggressively. In California, 4,711 nursing home residents had been infected and 663 had died by the end of April, about a third of all COVID-19-linked deaths that homes in the state have reported to authorities.
The KHN analysis is the first to compare Medicare’s public quality measures for the 198 California nursing homes that registered coronavirus cases by late April with the 983 homes with no cases reported to either the state public health department or Los Angeles County, where a majority of homes with infections are located. KHN found that California homes with coronavirus cases averaged 2.8 stars on Medicare’s five-star overall quality rating, while other homes averaged 3.5 stars.
On average, the homes that have had coronavirus cases had more complaints lodged against them and were fined 29% times more often. In addition, Medicare also calculated that their health violations of all types were 20% more serious. They also tended to be larger, averaging 105 patients versus 83 on the homes without virus cases.
The analysis found no substantial difference in the homes’ numbers of nurse aides or licensed practical nurses, but fewer registered nurses, who have the most medical training and supervise the other caregivers. On average, there was one registered nurse for every 39 residents at a California home without a patient coronavirus infection versus one RN for every 52 residents for homes with infections, KHN’s analysis found.
Certainly, nursing homes with stellar quality ratings also have had coronavirus outbreaks. Nursing Home Compare, the federal government’s consumer website, gave its top overall rating of five stars to Life Care of Kirkland, the Seattle-area nursing home that was the first reported to have a slew of infections. In California, 12 of the nursing homes with coronavirus infections had above-average ratings for both staffing levels and inspection results, although only three had no history of infection control citations.
The prevalence of coronavirus infections in lower-rated nursing homes could be explained by poorer care, but there might be other factors, said David Grabowski, a professor of health policy at Harvard Medical School. For instance, the lower-rated homes might be primarily located in low-income areas with high rates of coronavirus cases in those neighborhoods, he said.
“This suggests a very different set of policies if we want to protect nursing homes from further outbreaks,” Grabowski said.
Representatives of nursing homes rated as below average on Nursing Home Compare say that the coronavirus has thrown everyone off guard and that registered nurse staffing levels are irrelevant to whether a patient is infected by the new virus.
“It’s really hard to draw a straight line from” issues raised in previous years’ inspections “to this pandemic that even the experts didn’t see coming and were not prepared for,” said Elizabeth Tyler, a spokesperson for Longwood Management Corp., which runs three nursing homes with coronavirus infections that were also poorly rated before the pandemic: Studio City Rehabilitation Center, Burbank Healthcare and Rehabilitation Center and Sunnyview Care Center.
Burbank and Sunnyview have a health inspection rating of one out of five stars, which is much below average, while Studio City has two stars. Tyler said that health inspection ratings are a “very, very complex system” taking into account hundreds of different factors, and she hesitated to make any connections between past reviews or staffing levels and the current outbreak.
Lakeview Terrace in Los Angeles, which has recorded three cases of COVID-19, has been on a list of 15,000 nursing homes around the nation that health inspectors are required to visit more frequently because of repeated violations of patient safety rules. It has an overall Medicare rating of one of five stars — the lowest rating — and almost six times the national average of health deficiencies.
In August 2019, inspectors faulted the home after they saw a nursing assistant deliver a breakfast tray into an isolation room without putting on personal protective equipment. They also discovered the home was not keeping logs to track signs and symptoms of possible infections.
DJ Weaver, an administrator for Lakeview Terrace, said that on the rare occasion that mistakes happen, the facility counsels and trains staff and makes systemic improvements to prevent future occurrences.
“Overall, we have done a good job not allowing cross-contamination of any infectious organisms, which is the real danger,” Weaver said in an emailed statement.
Lakeview’s cases came as a result of accepting a hospital patient who had undiagnosed COVID-19, Weaver said. His infection of two roommates couldn’t have been prevented by the facility’s policies designed to protect residents from the virus. Those include banning staff from working at multiple nursing homes and suspending group dining and activities.
“That kind of thing is really hard to foresee,” Weaver said.
Jennifer Newbery entered the Rehabilitation Center of Santa Monica in April 2019. Up until the day of the video conversation, Jorge Newbery said he and his four siblings had been told by staff that the nursing home had only three cases of COVID-19, and that everything was under control.
But after the home transferred Jennifer Newbery to a local hospital, doctors told her family she tested positive for the coronavirus and had pneumonia, Newbery said.
When Newbery later called to thank the staffer for facilitating the video chat, he asked if the facility had seen any deaths.
The staffer said yes, Newbery recalled, and it floored him. “We absolutely had no idea,” he said.
Newbery said his mom is getting better at UCLA Medical Center Santa Monica. After she’s discharged, Jorge wants to take her to Chicago to live with him and his family.
Newbery said he had been unaware of Medicare’s critical assessment of the Rehabilitation Center, which has two stars out of five overall on Nursing Home Compare, denoting below-average care. Inspection records show that during a visit in May 2019, health inspectors faulted it for failing to sanitize a blood pressure cuff before it was used on a second patient, and for allowing a urinary drainage bag attached to a catheter to be touching the floor. In August 2019, inspectors determined the home violated California’s minimum staffing requirements because it lacked enough nurse assistants on 10 out of 24 days.
Huang, the administrator, noted Medicare gave the facility five stars, the best rating, in a quality category that assesses things like the frequency of patient trips to the hospital or emergency room and homes’ self-reported assessments of how often residents improved during their stays. The regulators who issued the May 2019 deficiency found no evidence of harm to a resident, he said.
Michael Connors, an advocate with the California Advocates for Nursing Home Reform, said nursing homes with fewer staff members and poor compliance with infection control practices are ripe for the spread of the virus.
“No place could be more dangerous to live right now,” Connors said. “It’s these characteristics that make nursing homes ground zero for COVID-19 outbreaks and deaths.”
-
Cue the debunking: Two Bakersfield Doctors Go Viral With Dubious COVID Test Conclusions
ByBarbara Feder Ostrov, CalMatters
 They dressed in scrubs. They sounded scientific. And last week’s message from two Bakersfield doctors was exactly what many stuck-at-home Americans wanted to hear: COVID-19 is no worse than influenza, its death rates are low and we should all go back to work and school.
They dressed in scrubs. They sounded scientific. And last week’s message from two Bakersfield doctors was exactly what many stuck-at-home Americans wanted to hear: COVID-19 is no worse than influenza, its death rates are low and we should all go back to work and school. Drs. Dan Erickson and Artin Massihi, who own urgent care centers in the region, had called a press conference to release their conclusions about the results of 5,213 COVID-19 tests they had conducted at their centers and testing site. They claimed the results showed that the virus had spread further in the area, undetected, and thus wasn’t all that dangerous.
But public health experts were quick to debunk the doctors’ findings as misguided and riddled with statistical errors — and an example of the kind of misleading information they are forced to waste precious time disputing.
The doctors should never have assumed that the patients they tested — who came for walk-in COVID-19 tests or who sought urgent care for symptoms they experienced in the middle of a pandemic — are representative of the general population, said Dr. Carl Bergstrom, a University of Washington biologist who specializes in infectious disease modeling. He likened their extrapolations to “estimating the average height of Americans from the players on an NBA court.” And most credible studies of COVID-19 death rates in reality are far higher than the ones the doctors presented.
“They’ve used methods that are ludicrous to get results that are completely implausible,” Bergstrom said.
Still, the early media coverage went viral. A local television report on the Bakersfield doctors’ press conference garnered more than 4.3 million views on YouTube. Elon Musk, the Tesla founder who wants to reopen his Fremont manufacturing plant this week, praised the doctors to his 33 million-plus Twitter followers. Tonight, the doctors are to get a conservative national audience for their views on Fox News, appearing on Laura Ingraham’s show.
In a rare statement late Monday, the American College of Emergency Physicians and the American Academy of Emergency Medicine declared they “emphatically condemn the recent opinions released by Dr. Daniel Erickson and Dr. Artin Messihi. These reckless and untested musings do not speak for medical societies and are inconsistent with current science and epidemiology regarding COVID-19. As owners of local urgent care clinics, it appears these two individuals are releasing biased, non-peer reviewed data to advance their personal financial interests without regard for the public’s health.”
The doctors had set up Bakersfield’s only private walk-in COVID-19 testing site and performed about half of all tests conducted in the area. They did not respond to a CalMatters request for comment Monday.
Misinformation thrives in a pandemic, and public health officials in California and elsewhere just can’t keep up.
“This pandemic has been so severely politicized in this country that evidence, no matter how poor, gets amplified enormously if it benefits one side or another,” said Bergstrom, who also was one of the first experts to critique the doctors’ study on Twitter. “We always hoped this crisis wouldn’t come, but that if it did we’d all be in this together. That’s been a huge surprise for all of us doing infectious disease epidemiology. It’s amazing to have to deal with this misinformation that’s being spread around for political purposes and the ways that interferes with adequate public health response.”
California Democratic state Sen. Richard Pan, a pediatrician who chairs the Senate Health Committee, said lawmakers who favor reopening the state had not yet cited the Bakersfield doctors’ conclusions as a justification to do so. But if they did, they’d “be on pretty weak ground,” he said.
The doctors “basically hyped a bunch of data and weren’t transparent about their methods. And they really played on the fact that they’re physicians. I think it’s quite disingenuous of them.” Pan said. “Then we have to push back on any media that promotes this information. They’re really doing this as a way to fish for attention.”
A Kern County public health spokeswoman told reporters that officials did not support the doctors’ call to reopen the region. Other epidemiologists echoed that sentiment.
But already the Bakersfield doctors — who tout their support of President Donald Trump and refuse to wear masks in public — had become heroes on social platforms and conservative media outlets, with some commenters calling them “brave.” Others who support continuing to shelter-in-place described the doctors as self-promoters whose chain of urgent care centers would benefit from reopening. Non-COVID medical visits have plummeted during the pandemic, endangering the practices of many doctors.
“As struggling business owners, their economic frustration is understandable. But it can’t be mistaken for science. People trust doctors,” Michigan emergency room doctor Rob Davidson wrote on Twitter. “When they tell Fox viewers to ignore recommendations from real experts, many will believe them…The impact of rejecting science-proven recommendations in exchange for these erroneous ideas would overwhelm health systems and cost lives. While re-opening the economy might be good for their Urgent Care Centers (sic), it would kill medical personnel on the actual front lines.”
Other highly-publicized studies of antibody test results by Stanford and USC researchers were similarly criticized for sampling bias and for the poor reliability of the tests it used. Researchers had suggested that COVID-19’s true spread in the community was much higher than expected and resulting death rates were low. But again, politicians and media who favor reopening states right away cited them as supporting evidence.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Cut Farmworker Pay During the Crisis? Don’t Do It, California Growers Say
By Kate Cimini, The Salinas Californian
 The Trump administration is considering cutting the pay of guest visa farmworkers during the coronavirus pandemic to help the farm industry. But California growers aren’t thrilled: They say it won’t help them much with their financial crisis. And they worry that it might even hurt them by creating uncertainty for their essential employees, prompting them to look elsewhere for work once the pandemic ends.
The Trump administration is considering cutting the pay of guest visa farmworkers during the coronavirus pandemic to help the farm industry. But California growers aren’t thrilled: They say it won’t help them much with their financial crisis. And they worry that it might even hurt them by creating uncertainty for their essential employees, prompting them to look elsewhere for work once the pandemic ends.Unions and other worker advocates also worry that reducing farmworkers’ wages would cause hardships for people already living on the edge of poverty, and may end up lowering the pay of domestic farmworkers, too.
Hugo Marcos has an H-2A visa, which allows growers to temporarily employ guest workers from other countries when there is a shortage of U.S. workers willing to take the jobs. He spends his days cutting hearts of romaine lettuce for Foothill Packing, Inc., and returns around 6 p.m. to the motel where he will stay for months.
Marcos just arrived in Salinas, but this is his fourth year working U.S. fields on an H-2A visa. He has earned enough to build a two-bedroom home in the Mexican state of Michoacan, and take care of his wife and two children.
(Image: Norcal harvesting fieldworkers pick strawberries early morning on March 31, 2020. Photo by David Rodriguez, The Salinas Californian)
“Trabajar de campo es complicado y especializado,” he said. In English: “farmwork is complicated and specialized.”
It took Marcos a long time to learn the skills he has: cutting the lettuce in a perfectly flat swipe to maintain a uniform look and size, then removing excess leaves and handing the heart off to be packaged right there in the field.
More than 257,000 people worked in the U.S. on an H-2A visa in 2017. These workers have been deemed essential during the coronavirus pandemic by county, state and federal government regulations.
In California, H-2A workers earn $14.77 an hour this year, or about $118.16 for an eight-hour day, one of the highest in the country for these workers. The average wage of an H-2A farmworker, known as the “adverse effect wage rate,” or AEWR, is based on a survey of growers and farm labor contractors, and the AEWR varies state to state.
For the same labor in Mexico, Marcos said, he would earn 70 pesos an hour, something like $23.28 a day. A drop in pay would reduce his children’s quality of life, he said. “Reduciría en nivel de vida que les damos,” he said.
Yet the Trump administration’s Department of Agriculture is exploring cutting H-2A worker pay, according to an NPR report. NPR found that “new White House Chief of Staff Mark Meadows is working with Agriculture Secretary Sonny Perdue to see how to reduce wage rates for foreign guest workers on American farms.”
The USDA declined comment on whether it is considering such a change, or how it would be accomplished. The administration could announce a temporary rule change, order a new rulemaking or issue an executive order.
“During these difficult times, President Trump and Secretary Perdue are doing everything to ensure farmers have the tools to carry out the vital work of feeding the American people,” a USDA spokesman told The Californian.
By cutting worker pay, the administration hopes to keep farmers afloat through the pandemic.
Without the wage cut, researchers expect to see up to a $688.7 million decline in sales, leading to a payroll decline of up to $103.3 million between March and May of 2020.
The pandemic has shut down restaurants, schools, cafes and other regular buyers of wholesale goods, leaving farmers hauling larger loads to food banks when they can afford to, and letting food rot in fields when they can’t.
As the administration contemplates cutting pay to workers on the frontlines, farmers also may be on the verge of receiving a $16 billion bailout to keep their operations going.
But agricultural industry representatives and workers’ advocates alike say the move to cut worker pay won’t solve the food-supply-chain crisis.
“To see wages being depressed would be reason for concern and evaluation,” said Chris Valadez, president of the Grower-Shipper Association of Central California, which represents more than 300 companies. “We are one of the few industries still essential, still open for business.
“Longer term, it should cause us to reevaluate the AEWR system and what goes into it, but right now, I just think it would create more uncertainty in the mind of the employees,” Valadez said.
Union officials say a pay cut for the temporary visa workers may reduce the pay of domestic workers, too, because the H-2A pay rate is considered the average pay for all farmworkers.
“To reduce their wages at any time would be of deep concern, given that many farmworkers are struggling to feed their own families,” said Gieve Kashkooli, the political and legislative director with the United Farm Workers, a union that serves domestic and foreign farm laborers. “It would be an even deeper concern to do that during this COVID crisis while the federal government has declared farmworkers essential. And it’s a total insult to them.”
Workers already underpaid, report says
According to the Economic Policy Institute (EPI), a nonpartisan think tank, H-2A workers are already underpaid compared to other workers.
“In 2019, the average wage of all nonsupervisory farmworkers was $13.99 per hour, according to USDA, while the average wage for all workers in 2019 was $26.53 per hour, meaning the farmworker wage was just 53% of the average for all workers,” read an EPI post. “And the average wage for production and nonsupervisory nonfarm workers—the most logical cohort for workers outside of agriculture to compare with farmworkers—was $23.51.
 “In other words, farmworkers earned 60%—just three-fifths—of what production and nonsupervisory workers outside of agriculture earned.”
“In other words, farmworkers earned 60%—just three-fifths—of what production and nonsupervisory workers outside of agriculture earned.”Anne Lopez, director of the Center for Farmworker Families, called it “un-American” to consider cutting wages during a health and economic crisis.
“They’re already impoverished,” said Lopez. “They live on the edge of survival, they have no guarantees. Right now they’re going through one of the worst periods I’ve ever seen…and to make things worse for them by cutting their pay? It’s obvious our president doesn’t consider these people as human beings.
“I think a lot of it’s racist, it’s classist, it’s to keep them where they’re at so they can’t progress. That’s why I say it’s un-American.”
Casey Creamer, president of the California Citrus Mutual, which represents 2,500 family citrus growers, said that although he had not seen a proposal from either the USDA or the Trump administration to cut H-2A wages, his group does not support cutting salaries of pickers.
(Image: Farmworkers Juan Manuel Virgen, left, and Daniel Lopez Avilez, middle, wear bandanas to protect them from then coronavirus and dust while they work in the fields of Salinas. Photo by David Rodriquez/Salinas Californian)
“It’s not a political reality, it’s not supportive of our employees that we have in place. It’s just not a thing that we do,” he said.
‘Not the most significant tool’
Some industry representatives say the move to cut wages is detracting from the ultimate problem: a sudden drop in demand.
In the Ventura-Santa Barbara area, citrus growers are leaving lemons on trees, Creamer said. Unlike other produce, which can be disked straight back into the ground and used to fertilize the soil, citrus must be harvested or it will endanger next years’ crop.
“We can hold for a little bit longer and hope that restaurants open back up,” said Creamer. “Growers will have to pay to come back in and harvest to drop food back to the ground. We’re buying some time right now but it can’t go on much longer.”
Valadez said that if the administration wants to help growers, it should “put enough money in the system so employers can pay workers.”
“I know if the food service market is down, it’s down, and there’s nothing we can magically do to change that,” he said. “However, where federal stimulus is focusing on direct payments, we also need to focus on purchasing power to get that food into the hands of people that need it.
“Lowering the AEWR is a tool but I don’t think it’s the most significant tool right now,” he said.
Valadez suggested an injection of funds into purchasers still buying food, particularly ones seeing a real upswing in customers, such as food banks.
Hunger is a problem across California, and Monterey County has one of the highest rates of food insecurity in the state. A 2016 report by the Monterey County Health Department placed the percentage of food-insecure people in the county at 34%.
At the Monterey County Food Bank, which typically serves 20% of the county’s adult population and 25% of its children, the number of people standing in line at the food bank has basically doubled, said the nonprofit’s executive director, Melissa Kendrick.
Many of those who take advantage of food banks are farmworkers themselves.
A food crisis
Some industry experts say without significant intervention, the farming landscape will be forever changed.
“We’re in a different world right now,” said Valadez. “As we move forward we might see a lower demand. That is extremely impactful to the industry and to the backbone of the industry: the workers.”
“Does going back to AEWR save the day?” asked Valadez. “I don’t know. Before COVID, I probably had an interesting quip to give you, but during this crisis I think there are other things that are more in-demand in the moment. Businesses need buyers for their product.
“We have to keep the system moving. Afterwards, we can have our debates and our cuts. But we have to keep the system moving.”
Some H-2A workers said they would still participate in the program even if wages went down, as they would make far more in the U.S. program than they would doing the same work in Mexico. Still, they said, it would be a blow to their finances and their plans.
Marcos has worked cutting romaine hearts for two years for Salinas-based Taylor Farms and two for Castroville-based Ocean Mist.
As Marcos washed up for dinner at a plastic washstand in the motel parking lot, pumping the water in bursts with his foot and lathering up with industrial green handsoap, he talked about his sons, the oldest, 8 years old, named for him.
They’re getting older, he said in Spanish, and he and his wife want to add a bedroom onto their blue-and-white home in Mexico so they could have their own rooms.
If his salary were to drop, Marcos said, it would hit his family hard. They would have to put construction plans on hold, probably for years.
“Suerte, pues, gracias a dios nos da la oportunidad venir por acá y lo aprovechamos después,” said Marcos.
“It was luck. Thank God I had the opportunity to come here. I made the most of it.”
Kate Cimini is a journalist for The Salinas Californian. This article is part of The California Divide, a collaboration among newsrooms examining income inequity and economic survival in California.
-
Facing Defiant Counties and Churches, Newsom Willing to Bend
Updated May 25, 2020.
 By Ben Christopher
By Ben ChristopherWith counties, cities, sheriffs, churches and now the President of the United States challenging Gov. Gavin Newsom’s authority to maintain restrictions over business and public life in the face of the ongoing pandemic, the governor has perfected an approach: Speak collaboratively and carry no stick.
“This process has been remarkably collaborative,” he insisted today, downplaying resistance to the statewide shelter-in-place order in effect since March 19. “There are a few examples that are exceptions in the state of California that tend to get highlighted disproportionately, but I just want to express this: they are exceptions.”
(Image: File photo by Anne Wernikoff for CalMatters)
What about, say, the Tulare County Board of Supervisors’ recent vote to allow movie theaters, nail salons and sit-down restaurants to open this week, in defiance of state restrictions? The governor called that “a dynamic that will work itself out.”
“This is again an exception. The overwhelming majority of counties are working very, very collaboratively. I don’t wake up to look to be punitive.”
Since the early days of the pandemic, Newsom has been much more comfortable imposing his statewide order through public warnings, badgering, and guilt-tripping. When sun-seekers flocked to beaches in Orange County, he ordered them shuttered. He has yet to send in the National Guard to round up wayward surfers. Though businesses that reopen prematurely have been threatened by state licensing boards, few have been punished.
But whether or not the governor is looking for a fight, he may get one.
Today President Donald Trump called upon places of worship across the country to open their doors immediately. The president also declared his intention to “override” state governors who stand in the way, though it is unlikely he has that authority.
With his announcement today, Trump is taking sides on a standoff in California, where more than a thousand churches declared their intention to reopen this weekend in defiance of state and county orders. This came after the federal Justice Department wrote a letter warning Newsom that “the Constitution calls for California to do more to accommodate religious worship.”
Some religious leaders in the state have argued that religious services are essential to the emotional and spiritual well-being of their congregants — and that houses of worship can and should be entrusted to enforce social distancing protocols. The state has instead prohibited worship gatherings “while exempting a laundry list of industries and services purportedly ‘essential’ to the government’s various interests, including medical cannabis dispensaries and other medical providers, courts, public utilities, daycare and childcare, and ‘necessary’ shopping,” the South Bay United Pentecostal Church in Chula Vista wrote in its recent lawsuit challenging the state.
Later in the day, a federal panel of the 9th Circuit Court of Appeals sided against the churches and with Newsom. “We’re dealing here with a highly contagious and often fatal disease for which there presently is no known cure,” the majority wrote, citing an earlier justice’s observation that if a court fails to “temper its doctrinaire logic with a little practical wisdom, it will convert the constitutional Bill of Rights into a suicide
pact.”The sole dissenting judge on the panel noted the churches had provided a list of measures they would willingly put in place upon opening — including spacing out seating, requiring masks, and banning singing, hugging, hand shakes and hand-holding. He regarded the ban on religious services as “inflexible and overbroad.”
To date, there have been at least 20 private lawsuits challenging some aspect of the state’s response to the pandemic — with at least four filed by churches and other religious institutions.
Newsom urged patience, noting that his office is in the process of producing new rules for houses of worship that will be released on Monday “at the latest.” (Update: As promised, the state’s Department of Public Health issued new guidelines on Monday that will allow Californians to gather at places of worship under strict social distancing guidelines that limit “attendance to 25% of an area’s maximum occupancy – or up to 100 attendees.” The new rules also apply to political protests. The Department also announced that retail shops may open for in-store shopping under strict rules. Retailers in some counties had already been granted the right to do so. The new rules apply statewide.”)
“We are looking forward to a very positive working relationship with faith leaders as we make public those documents and look forward to working through this issue in the spirit of cooperation and collaboration.”
On paper, the governor’s emergency powers are shockingly broad. But since the beginning of the public health emergency, Newsom has had to strike an awkward balance between what he is legally allowed to do and what cities, counties and California’s citizens are willing to swallow.
“This ‘bend but don’t break’ approach has worked for him so far,” said Dan Schnur, a political science professor at the University of Southern California and UC Berkeley, and political communication guru for Republican presidential and gubernatorial candidates. “As long as Newsom can find a way to give locals a little bit of leeway in exchange for them not moving as aggressively as they might prefer he avoids a political problem, but much more importantly, he lessens the risk of a pronounced spread of the virus.”
Last week, Newsom revised the state’s benchmarks that counties must meet before they can ease their local restrictions further, effectively lowering the bar for restaurants, barber shops and shopping malls across the state to reopen. That came after county officials in Southern California floated the idea of banding together to create their own looser set of guidelines. Newsom has said that the relaxing of the state rules was guided by public health data and not political pressure.
Some counties have “little to no spread, no cases, and that’s why these variances are appropriate,” he said today.
But the move may also be an acknowledgment that the governor’s power is restricted, if not by the state constitution, then by his own limited appetite for escalation.
That was put to the test when Tulare County’s supervisors voted to broadly reopen despite not having met criteria the Newsom administration established for counties to do so. The red county in the Central Valley has the sixth-highest COVID-19 hospitalization rate of any California county, according to a CalMatters tracker, and 73 reported deaths.
In an uncharacteristic bit of hardball from this administration, the governor’s Office of Emergency Services director Mark Ghilarducci wrote the county warning that the move “could threaten Tulare County’s eligibility for disaster funding.”
“We certainly interpret their letter as an intent to withhold funding to Tulare County,” said Jason Britt, the County Administrative Officer, when asked by email. “We hope we can arrive at an amicable solution with the state.”
Asked about it today, Newsom certainly struck an amicable tone.
“I want to be responsible and respectful to the deep economic challenges that all of us are facing,” he said. “I want to reflect a…sense of empathy and understanding to those that have disagreements and respect, but hope that they know we look forward to working with them.”
The Tulare resolution is only the latest bit of pushback the governor has received from impatient Central Valley elected leaders.
On May 16, Merced County Sheriff Vernon Warnke announced that he and his department would not be enforcing violations of shelter-in-place.
“I truly believe that Governor Newsom’s motivation is to have the majority of the citizens (and illegal residents) dependant on governments (sic) assistance so he could maintain this control once this ‘pandemic’ is declared over,” the Sheriff’s office posted on Facebook, adding a Trumpian flourish: “The CURE should not be worse than the disease.”
A day earlier, the city council in Atwater, also in Merced County, engaged in a bit of trolling-by-municipal-resolution, declaring the town a “sanctuary city for all businesses” hoping to operate despite any public health directive.
This all follows a headline-grabbing stand-off earlier this month between public health authorities in Alameda County and Tesla founder, Elon Musk. After the Bay Area billionaire opened up the car company’s Fremont factory, daring authorities to arrest him and then suing the county, Newsom again adopted a conflict-averse response.
“It’s not heavy-fisted — or heavy-handed rather — or close-fisted,” he said at a press conference earlier this month. “We will continue to work as collaborative as possible.”
Musk has since dropped the suit.
Newsom is juggling competing public anxieties. The most recent polls, from April, found that roughly 70% of Californians surveyed said they approved of Newsom’s handling of the public health emergency. Similar numbers expressed concern that relaxing public health mandates too soon could trigger another out-of-control outbreak.
Today, the governor said the state has approved 43 applications from counties hoping to move forward with accelerated reopening plans. Two more approvals are expected by the end of the day.
-
Financial Help for California’s Undocumented Immigrants Starts Monday
By Jacqueline García, La Opinión
 California’s undocumented immigrants can begin applying Monday for disaster relief payments of up to $1,000 per household under Gov. Gavin Newsom’s coronavirus emergency assistance plan.
California’s undocumented immigrants can begin applying Monday for disaster relief payments of up to $1,000 per household under Gov. Gavin Newsom’s coronavirus emergency assistance plan.In April, Newsom announced a one-time, $75-million fund for undocumented adults who are not eligible for other forms of government assistance, such an unemployment benefits and federal stimulus checks. A qualifying undocumented adult can receive $500, with a maximum of $1,000 per household.
Since the announcement was made, many undocumented immigrants have been waiting for information to apply as soon as the application period opened.
California has more than two million undocumented immigrants. Nearly one in ten workers is undocumented.
With the funds spread among so many people, most families will not receive the funding. Applications are approved on a first-come, first-served basis, until the money runs out.
“In the best case scenario, these funds would reach one in 10 people,” said Unai Montes-Irueste, director of communications with United Ways of California.
Magdalena, 47, an undocumented essential worker who up until recently worked making face masks in a sewing factory, hopes to receive the assistance.
“I haven’t worked for about a week because my 74-year-old mother became ill and we don’t know if she has the coronavirus,” said Magdalena, who preferred not to give her last name because of her undocumented status.
Magdalena said if she receives help from the state government, she could close the gap on her lack of income, which affects her family of four.
“This money would help me pay the rent,” she said.
Another possible beneficiary is Julio Peralta, 45, a single father of a 16-year-old son and a 12-year-old daughter with spina bifida.
Peralta said that none of them has a legal status in the country since they arrived in Los Angeles from Guatemala five years ago in hopes of obtaining a cure for his daughter.
“But right now with the pandemic, I already fell behind on my rent payments for April and May,” said Peralta, who is not working.
Peralta said if he receives the financial aid from the government, he would use the money to find a place to live in Los Angeles since his daughter is receiving treatment at the Children’s Hospital Los Angeles
“But I don’t know how it is applied,” he said.
The process of applying
Montes-Irueste of United Ways of California — which has helped undocumented immigrants without bank accounts during the pandemic — said it is important for people to know where to get help and avoid being scammed.
Called the Disaster Relief Assistance for Immigrants Project, the $75 million in state funding will be distributed to 12 organizations throughout California.
Additionally, the governor said $50 million would be available from philanthropy groups to be supervised through the organization Grantmakers Concerned with Immigrants and Refugees (GCIR). However, as of Thursday, only $13 million had been collected from philanthropy through immigrantfundca.org.
The organizations were selected from among Immigration Services Financing contractors who have existing agreements with the state. The state Department of Social Services also selected nonprofits that have the ability to provide a high volume of application assistance services to undocumented populations in specific geographic locations.
Applications will be available until funds for each region are exhausted.
Eligibility
An applicant must be undocumented, over 18 years of age, ineligible for federal assistance related to COVID-19 such as the stimulus check or unemployment benefits, and able to demonstrate that they have faced financial difficulties as a result of the pandemic.
Organizations will verify the applicant’s documents to ensure they match the information provided and will make the final decisions.
To apply, undocumented immigrants should contact the group representing their area:
Northern California:
California Human Development Corporation
(707) 228-1338 www.californiahumandevelopment.org/
Covering Alpine, Amador, Butte, Calaveras, Colusa, Del Norte, El Dorado, Glenn, Humboldt, Lake, Lassen, Mendocino, Modoc, Napa, Nevada, Pleasure, Plumas, Shasta, Sierra, Siskiyou, Solano, Sonoma Tehama, TrinityBay Area:
Catholic Charities of California
Alameda and Contra Costa: www.cceb.org
Marin, San Francisco, San Mateo: www.catholiccharitiessf.org/
Santa Clara: www.catholiccharitiesscc.org/Central Coast:
Mixteco / Indígena Community Organizing Project (MICOP)
www.mixteco.org/drai/3
Santa Barbara: (805) 519-7776
Ventura: (805) 519-7774Community Action Board Santa Cruz
(800) 228-6820 www.cabinc.org/
Covering Monterey, San Benito, San Luis Obispo, Santa CruzCentral Valley:
United Farm Workers Foundation (UFWF)
(877) 527-6660 www.ufwfoundation.org
Covering Ash, Kern, Kings, Wood, Merced, Tulare and MonoCalifornia Rural Legal Assistance Foundation (CRLAF)
(877) 557-0521 www.crlaf.org/drai
Covering Mariposa, Sacramento, San Joaquin, Stanislaus, Sutter, Tuolumne Yolo and YubaLos Angeles and Orange County:
Asian Americans Advancing Justice
(213) 241-8880 www.advancingjustice-la.org
Coalition for Humane Immigrant Rights (CHIRLA)
(213) 201-8700 www.chirla.org
Los Angeles Central American Resource Center (CARECEN)
(213) 315-2659 www.carecen-la.org/Inland Empire:
San Bernardino Community Service Center
(888) 444-0170, (909) 521-7535 www.sbcscinc.org
Covering Inyo, Riverside, San BernardinoTODEC Legal Center Perris
(888) 863-3291 www.TODEC.org
Covering Inyo, Riverside, San BernardinoSan Diego and Imperial County
Jewish Family Service of San Diego
Imperial County: 760-206-3242
San Diego County: 858-206-8281Jacqueline García is a reporter with La Opinión. This article is part of The California Divide, a collaboration among newsrooms examining income inequity and economic survival in California.
-
For Some California Teens, School Closures Led To Work In The Fields

By Elizabeth Aguilera, Cal Matters
Updated June 22, 2020
Sisters Maria and Jennifer Salvador start their days before the sun. The Southern California teenagers report to work at an Oxnard strawberry farm with one goal: To harvest as many bright red strawberries as they can.
Each 20-pound box of stemless strawberries they collect brings in $3.
In the evenings when school was still in session, albeit remotely – and after chores at home were done — Maria and Jennifer turned to their school work. The two relied primarily on their father’s cell phone because the school district’s hot spot didn’t work in their Oxnard neighborhood.
“It has gone badly for me,” said 16-year-old Jennifer about remote learning. “It’s not the same because it’s difficult to know how to do the work that the teachers send. You can’t ask questions. It’s like being all alone.”
(Image: Sisters Maria (left) and Jennifer Salvador of Oxnard are two of the many California teenagers who worked in the farm fields to help support their family when their high school closed during the pandemic. In the evening, the sisters tried to do homework online and via email without the benefit of any direct instruction that took place digitally during the day. Elizabeth Aguilera for CalMatters.)
Like many students in California’s agricultural communities, the Salvador sisters’ personal and educational lives have been upended by the coronavirus pandemic When the health crisis interrupted education across the state, closing schools in March and moving learning online, many of these students went to work in the vast green fields that feed much of the country. Jennifer and her 19-year-old sister, for instance, missed out on live digital meetings with their teachers and small group meetings that took place while they were curved over strawberry plants, sifting for the ripest berries.
This poses a challenge for California schools whose migrant students fell behind this spring. As fall approaches, administrators and teachers are scrambling to figure out how school will look amid the ongoing pandemic — and how to help these students return to classes and catch up. Advocates worry some students could decide to continue working instead of going back to school if they feel they have lost their educational footing.
In Oxnard, where Maria and Jennifer are students, school district officials knew the fields would beckon students whose families already live on the economic edge.
“We absolutely saw this as an outcome of the school closure,” said Tom McCoy, assistant superintendent of educational services at Oxnard Union High School District. “We are working to make sure they have a chance to make up those classes and help them do that once we get set up again. It’s really about being as flexible as we can be to keep the kids connected with their schooling.”
McCoy said a committee is studying options, including making school viable for students who may need to work. The district is planning to extend office hours, and to require that digital meetings be recorded for later viewing. Shifting to a quarter system is also on the table, he said. Quarters allow students to take more classes overall but focus on three to four classes each quarter instead of six or seven throughout a semester.
Classes on weekends and evenings also may be offered, McCoy said.
So far, state-issued guidance for returning to schools focuses mostly on pandemic safety – social distancing and taking temperatures, for instance — rather than offering recommendations for how to support students who have fallen behind. The state Department of Education guidance outlines three possible models for bringing students back that include distance learning, in-class small group instruction and a hybrid of the two.
Advocates worry the virtual or hybrid models could keep students in the fields and affect their education long-term.
Statistics on how many students worked in the fields because of pandemic-related school closures are non-existent.
Federal regulations allow kids as young as 12 to work in agriculture as long as school is not in session. Those who are at least 16 and not enrolled in school can work any time.
 A U.S. Government Accountability Office report, released in 2018, found there were nearly half a million youth in the U.S. under 18 working in agriculture in 2016, including on their own family farms. California is home to the largest share of minors working as hired crop hands.
A U.S. Government Accountability Office report, released in 2018, found there were nearly half a million youth in the U.S. under 18 working in agriculture in 2016, including on their own family farms. California is home to the largest share of minors working as hired crop hands.Concerns about children working in agriculture during school is part of a larger issue. For decades, efforts have been made to raise the age limit because of the perils of pesticides, back-breaking work and dangerous equipment that has maimed or killed children.
“The law says students can’t work during school hours, but there are no hours going on right now so many of them are working,” said Kendra Moesle of the Association of Farmworker Opportunity Programs and Children in the Fields Campaign. “It’s really going to impact education because they are not focusing on school work and, secondly, there is the physical danger.”
(The Salvador sisters earned $3 for each 20-pound box of strawberries they picked. Photo by Elizabeth Aguilera for CalMatters)
The dilemma is playing out in agricultural communities from Imperial County on the southern border to Monterey on the Central Coast to Butte County in Northern California.
Students went to work because their parents’ jobs were lost or reduced or because parents got sick, said Yvette Irving, superintendent of the Gonzales Unified School District, in the Salinas Valley.
“Our migrant students don’t sit idle in the summer,” she said. “So this just expedited things and did not allow them to finish the semester of their high school program.”
Irving said her district’s priority is bringing the students back to in-person instruction, but it will provide distance learning for those who need it.
“We are concerned about getting them back on track in a traditional classroom setting with daily teacher-to-student interaction and making sure they have all the prerequisites they need to go on to college or a different aspect of the workforce,” Irving said.
The Gonzales Unified School District is in Monterey County, where a federally funded program for migrant students went into overdrive this year to reach migrant students when remote learning began, said Summer Prather-Smith, senior director of the Migrant Education Program Office.
Monterey County is home to the largest share of migrant students enrolled in the program in California, with more than 11,000 youths ages 3 to 21. But the program only supports students whose families move for work every three years. Many of the teens also work.
 Since March, counselors and case workers met with students, set up learning plans and provided late-night support. The program gave all students access to an online tutoring program and hired extra teachers to teach math in the evenings. Toward the end, like most students, the kids dropped off but the outreach will continue into summer and the new school year, said Prather-Smith.
Since March, counselors and case workers met with students, set up learning plans and provided late-night support. The program gave all students access to an online tutoring program and hired extra teachers to teach math in the evenings. Toward the end, like most students, the kids dropped off but the outreach will continue into summer and the new school year, said Prather-Smith. She said she is even more focused on how to lure students back to school and wants the district to offer quiet spaces for students to use for remote learning, much like a traditional study hall with social distancing.
(Carla Diaz, 16, works in the raspberry orchards in Oxnard with her mother. She went to work in the fields when schools closed and she did her schoolwork in the evenings to try to stay caught up. Photo by Elizabeth Aguilera for CalMatters)
“The longer they are disengaged from it the harder it is to ask them to go back,” she said. “We have to be more enticing than the money they are going to make.”
As an added challenge, a growing number of California’s farmworkers have come from indigenous communities, mostly in Mexico, who speak dialects including Mixteco. This can make it more difficult for families to engage with schools, said Arcenio Lopez, executive director of the Mixteco/Indigena Community Organization Project, an organization founded to help the indigenous farmworkers.
“Our students are not feeling like they will be able to enter the university or college and we are seeing a lot of emotions and stress and mental health issues,” said Lopez. “They are very stressed.”
Carla Diaz, 16, is from one of these families.
For her, schooling began once she returned home from the raspberry orchards in Oxnard where she toiled alongside her mother.
A couple of classes scheduled virtual meetings after 5 p.m. but mostly she communicated only by email — a wearisome task, as Mixteco is her first language, Spanish her second and she is learning English. But she did it, keeping an eye on her A average.
“I miss my teachers, I miss the extra counseling,” said Carla, who is the fifth of 10 children.
Her parents have little education, she said, and while they want her to have success they can’t help her with homeschooling.
“My mom says I have to work for a better future, because she doesn’t want us to suffer like they have,” said Carla. “They didn’t go to school and that’s why they work in the fields.”
Carla and the sisters are members of a youth group called Tequio, focused on getting kids from the fields to college and is run by the Mixteco/Indigena Community Organization Project.
The Salvador sisters vow to return to school but for now, they are the sole earners for their family of nine. Their mother had a baby just weeks ago and their father is caring for them.
With only their eyes showing above a bandana and below a baseball hat, they focus only on the strawberries, swooping their hands into plants to cut the berries with sharp metal tubes wrapped around their thumbs.
Older sister Maria can turn in 50, 20-pound tubs of strawberries a day; Jennifer aims for 30.
“I haven’t learned anything during this time, it’s very sad,” said Maria Salvador, who graduated from Hueneme High School on June 12. “It’s very hard to work in the fields. I want a better future.”
She hopes to enroll at Oxnard College in the fall.
-
Hearken Testin'
-
Here’s How Putting California’s Homeless in Hotels Actually Works
ByMatt Levin, CalMatters
 Richard Dobbs was coughing, feverish, and preparing to sleep on the sidewalk again.
Richard Dobbs was coughing, feverish, and preparing to sleep on the sidewalk again. Dobbs, 60 and homeless in Sacramento for the past two years, had just been discharged March 28 from Sutter Medical Center’s emergency department, where he was given a test for COVID-19, the disease caused by the new coronavirus, and written instructions for how to self-isolate while he awaited the results.
“Separate yourself from other people in your home,” read a bold-faced warning. “Stay home except to get medical care,” read another.
(Image: Richard Dobbs in his Sacramento motel room. Photo courtesy of Ginny Bayly, Loaves and Fishes)
Home for Dobbs most nights was the sidewalk next to the Wells Fargo Pavilion, a theater in downtown Sacramento. Staff at a local food bank saw him in line the next day and scrambled to find him a motel room where he could safely self-quarantine.
Dobbs’ test results came back negative. But with his motel stay scheduled to end on Monday and county caseworkers trying to place him in transitional housing, Dobbs is fearful he’s now even more vulnerable to the virus.
“I would stay (in the motel) for a while now because I’ve always hated going into shelters,” said Dobbs. “Because you get sick going into those places.”
In an unprecedented effort spurred by the pandemic, Gov. Gavin Newsom and local governments across the state say they are scrambling to find 15,000 hotel rooms for people like Dobbs: homeless and particularly susceptible to or exhibiting symptoms of coronavirus infection.
As homeless Californians begin to move into these units, new questions have arisen for hoteliers, shelter providers, health care workers and government officials: How much should a room cost, and who should pay for it? How will meals be delivered? How will residents with mental health and addiction issues be handled?
And, when all this ends, will people in these rooms end up back on the street?
Here are some answers:
How many homeless people have been moved into hotels so far, and how many rooms are available?
The data here is sketchy. A spokesperson from Newsom’s office said Thursday 1,813 hotels or motel rooms are now occupied as part of Project Roomkey, a joint effort between the state, counties and the Federal Emergency Management Agency. Newsom also said during a press conference that the state had helped procure 8,742 rooms.
State and local housing officials say Newsom’s numbers are underestimates because they don’t capture independent efforts from county governments to set up hotel rooms on their own. San Diego County, praised by Newsom for its quick action, secured 1,300 rooms in mid-March. The number of people actually relocated to hotel rooms is also due to increase significantly this week. Los Angeles County alone plans to have more than 1,069 beds occupied by the end of the week.
But the task ahead is daunting. More than 150,000 people are homeless in California, 108,000 unsheltered; an optimistic count of the number of those moved to hotel rooms so far represents a little over 1% of that total. The effort has already required a great deal of logistical gymnastics and staffing. Even focusing on only the highest-risks populations — seniors, those with underlying health conditions — will be a huge undertaking.
Where are the hotels? And are we talking about the Ritz or Motel 6?
State and local health officials have declined to share a comprehensive listing of hotels that have opened their doors to homeless people. They argue releasing such information risks those individuals homeless showing up at hotels and demanding rooms without referrals from physicians or caseworkers.
More than 1,000 hotels across the state have at least expressed an interest in providing emergency quarantine accommodations, although that includes temporary housing for health care workers and first responders, according to data from the California Hotel & Lodging Association. Hotels in Los Angeles, San Diego and Orange counties alone account for more than 40% of possible rooms in that survey.
While some higher-end boutiques and well-known brands such as Comfort Inn and Radisson are participating, state and county officials are having more success with smaller, independent motels that may already have relationships with local housing authorities.
That’s partly because independent motel owners can act quicker than major corporate chains, and partly because those motels are often already located in neighborhoods with shelters and other homeless service providers, making it easier for counties to get them up and running.
Are enough hotels willing to do this?
Yes, at least so far.
Local health and homelessness officials will tell you finding hotels and motels willing to participate hasn’t been a major bottleneck yet. At least not compared to other logistical hold-ups (see below).
“We have a lot of interest, a lot of receptiveness, from motel operators,” said Cynthia Cavanaugh, director of homeless initiatives for Sacramento County. “We actually have interest from places we never expected, so that part has not been as much of a challenge.”
The major reason hotels and motels are opening their doors so readily is the obvious one: It’s not like demand for hotel rooms is high right now.
“(These are) brutal, unprecedented, extraordinary times,” said Lynn Mohrfeld, president of the California Hotel and Lodging Association. “Anyone that is open right now is losing money,”
Mohrfeld said on a typical non-pandemic week, about 70% of hotel rooms across the state are occupied. Now it’s single digits.
Who is paying for the hotels, how much are they paying, and what about insurance?
Newsom said late last week that the Federal Emergency Management Agency will pick up 75% of the tab for rooms that are housing homeless people who have tested positive, are symptomatic, have been exposed to the virus, or are in highly vulnerable populations. Counties are on the hook for the rest, as well as for services, such as case managers and counselors, that residents may need. Counties can tap state emergency funds to help pay.
So far, the state has distributed $150 million to counties to help pay for motels and other homelessness services, but the total cost borne to taxpayers will undoubtedly be more.
Lease costs vary from county to county and hotel to hotel. But Mohrfeld said room rates in general are at least in shouting distance of the rates the federal government pays when its employees stay in California hotels. That “standard” rate is about $96 per room per night (higher in most cities), and leases are typically 60 to 90 days with options for extensions. Hotels may also be receiving additional reimbursement for higher insurance rates and associated costs.
While local governments and the state have generally agreed in contracts to pay for any property damage incurred as a result of repurposing hotel room, Mohrfeld said there’s still uncertainty among some hotel owners that their properties will be returned to them in the condition they were in before the quarantine.
“It’s the fear of the unknown,” said Mohrfeld.
Who gets into these hotels?
First priority for state and county health officials are homeless Californians who have tested positive or are experiencing symptoms of COVID-19.
While the process varies from county to county, the general timeline is as follows: Shelter staff identify someone with symptoms and quarantine them within the shelter as quickly as possible. The shelter staff then alert county health and homelessnsess staff that the individual is in need of a motel room where they can self-isolate. That person is then safely transported to an “isolation” motel where an on-site nurse and other medical staff monitor their health. Once the person is free of symptoms and believed not to be contagious anymore, they are discharged back into a shelter or into another housing option, if available.
If their condition worsens, they may be taken to a hospital. These “isolation” motels may include not only people who are homeless, but others who are symptomatic or have tested positive but lack a safe place to self-quarantine (those in senior homes, for example).
Multiple shelters across the state have already reported residents with positive tests, and officials are hoping to avoid outbreaks in congregate shelters. Removing symptomatic patients can also free up more beds for healthy people to come in off the streets. But some advocates still warn that congregate settings and resident turnover puts healthy people at risk of contracting the virus.
Those identified as symptomatic on the street will also be eligible for the hotels.
What about the homeless who don’t have the virus or aren’t symptomatic?
Homeless Californians over 65 or with underlying health conditions will be placed in their own motel rooms, separate from those who have tested positive or are symptomatic. It’s unclear how long this population will be allowed to stay in their rooms, and may vary from county to county.
In recent comments, Newsom has pushed back against any expectation that the state may be able to provide motels for every Californian living on the streets. The hope is that by rapidly expanding emergency shelters (San Diego has converted its convention center to a shelter; Los Angeles has converted city recreation centers), homeless individuals that don’t fit the “high-priority” populations eligible for hotels will still be able to come indoors.
But some homelessness advocates have decried that approach, insisting that hotel rooms be commandeered for anyone without shelter in the midst of a pandemic. A plan to convert San Francisco’s Moscone Center into a temporary shelter has been scaled back after photos emerged of a conference center packed with thin sleeping mats, folding chairs and not much else.
Why the delay between acquiring rooms and getting people inside?
On March 16, Newsom said the state had helped acquire its first two hotels for emergency homeless housing, by the Oakland Airport in Alameda County. But the ink on the lease had been dry for nearly two weeks before people who were homeless actually started to move in. Why the delay?
Staffing. Arranging physicians, nurses, caseworkers, food delivery, security, cleaning and other services has been more of a hurdle than actually acquiring the hotels. For hotels isolating those who are symptomatic, personal protective equipment is needed for county, nonprofit and hotel staff.
Transportation has also proved a challenging issue as counties grapple with how to safely move symptomatic homeless people with pets and belongings while protecting transit workers.
“Our population is not just getting on a bus with a suitcase,” said Cavanaugh. “The need to have specialized transportation to handle all of those things is large.”
Who is working at the hotels?
Staffing will vary from hotel to hotel and county to county, and will depend on whether hotels are intended for isolating homeless people suspected of having the virus or simply vulnerable because of age or underlying health conditions.
The Mayfair Hotel in downtown Los Angeles has 23 people who have COVID-19 symptoms or have tested positive, including several who are homeless. Eventually, the goal is to have 284 of the hotel’s 300 rooms occupied with people who are self-isolating.
There’s a nurse on site 24 hours a day. Physicians conduct telephone and video check-ins with residents. Private security monitors each floor, and private cleaning crews in personal protective equipment clean rooms when needed.
Either Stephen Fiechter or someone else from PATH, a nonprofit homeless service provider, is there all day to check-in with homeless residents on the phone, drop off meals at their door, and connect residents with shelter and other housing options once their stay is over.
Fiechter said that while organizations like PATH are happy to assist with the motel initiative, it’s been difficult to maintain their other homeless operations at the same time, which include operating shelters.
“It’s the staffing piece that’s really challenging,” said Fietcher. “Bringing on experienced folks, but not stripping our other programs.”
While not the case at the Mayfair, hotel staff may also be deputized to assist in cleaning up rooms or common spaces.
Mohrfeld, head of the statewide California hotel association, said that while some custodial workers may be hesitant to help, others are eager for the work and feel a sense of civil mission.
“Some are okay with it, some are fearful — it kind of runs the gamut,” said Mohrfeld, who said some hotels are negotiating with counties to ensure their staff receive protective gear.
What happens after the virus threat subsides?
While hotel owners, state and local officials, and homelessness advocates are understandably focused on the public health crisis at hand, the question of what will happen to the homeless after the virus threat subsides lingers.
Newsom has said many of the leases the state is negotiating include an option to purchase the entire property for more permanent housing, But Mohrfeld said that most hotels and motels he’s been in contact with haven’t agreed to such options.
While the optics of eventually forcing homeless people out of a hotel room may be a public relations nightmare, Mohrfeld said he’s more concerned with possible future litigation from advocates preventing such action if better housing options don’t materialize.
“What happens when they don’t have anywhere to go and… (advocates) sue the state and say they can’t move them and then the state’s hands are tied?” said Mohrfeld. “The litigation aspect concerns me a lot.”
Homeless service providers are still trying to connect residents in shelters, motel rooms, and on the street to more permanent housing solutions.
“None of this is stopping our attention from what really resolves homelessness, and we think we will have an opportunity to move folks into permanent housing,” said Emily Halcon, homelessness services coordinator with the city of Sacramento.
What about neighbors of these hotels?
How do neighbors feel about nearby hotels housing dozens of homeless people, some with COVID-19 symptoms? In Orange County, a senior community next to a 138-bed hotel slated to house the homeless protested the arrangement until the county agreed to find another site.
But other than that high-profile example, Mohrfeld said complaints from neighbors have been relatively rare and haven’t interfered much with motels agreeing to leases.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Housing, Homelessness Funds Mostly Spared in Proposed Budget cuts
ByMatt Levin, CalMatters
 With a forecasted deficit of near-record proportions and an economy in freefall, homelessness and low-income housing advocates were braced for painful cuts in the revised budget proposal Gov. Gavin Newsom unveiled Thursday.
With a forecasted deficit of near-record proportions and an economy in freefall, homelessness and low-income housing advocates were braced for painful cuts in the revised budget proposal Gov. Gavin Newsom unveiled Thursday. But unlike some of the more severe pandemic-induced rollbacks Newsom outlined in areas like education and climate change, affordable housing and homelessness dollars were mostly spared from the administration’s fiscal cleaver.
Given an assist from the federal government’s March stimulus package, Newsom is proposing $750 million to buy hotels and motels currently used for emergency homeless housing, hoping to turn the properties into more permanent solutions. Another $500 million in tax credits for building low-income housing was preserved from Newsom’s pre-pandemic budget plans — a major win for affordable housing developers as they try to fill the state’s shortage of 1.3 million low-income homes.
(Image: LA County is working with state, federal and local partners on Project Roomkey, an initiative to bring medically vulnerable people experiencing homelessness indoors during the COVID19 pandemic. Photo by Michael Owen Baker, County of Los Angeles via Flickr)
“We are very encouraged to see the governor continue to prioritize housing and homelessness resources,” said Chris Martin, legislative advocate for the nonprofit advocacy group Housing California.
But while Newsom’s housing and homelessness budget was rosier than some had expected, the proposals still leave unanswered difficult questions that state lawmakers and the governor will have to settle before their June 15 constitutional deadline to pass a balanced budget:
- How many hotels and motels can be realistically transformed to permanent housing, and where will funding for services come from?
- What will the state do about the mounting levels of missed rent payments piling up for renters and landlords?
- What happens when federal emergency dollars dry up?
“A lot more needs to be done,” said Assemblyman Miguel Santiago, Democrat from Los Angeles, who has proposed legislation, backed by big-city mayors, to spend $2 billion annually for shelters, permanent housing and homeless services.
“At the end of the day, does it make sense to move at a breakneck speed to house thousands of people during the emergency phase of the pandemic, and then throw everyone out on the streets when it’s over?”
Here’s what else you need to know about Newsom’s housing and homelessness budget in a pandemic-induced recession.
What was proposed before we talked about “bleach injections“
Before phrases like “social distancing” and “mask hoarding” entered the day-to-day lexicon, Newsom staked much of his political capital on fixing the state’s painfully visible homelessness woes. His January budget included a one-time infusion of $750 million in new state homelessness dollars, the most California had devoted to the issue in recent memory. It also proposed a new system of bypassing local governments to deliver those dollars directly to homeless services providers, along with hundreds of millions to reform the state’s low-income health insurance program to pay for things like housing and addiction services.
Another item Newsom put forward: an additional $500 million in tax credits for low-income housing developers. In his February State of State address, Newsom even flirted with broader ambitions laid forth by his homelessness task force, including ongoing homelessness spending housing providers could rely on every year.
What’s been tossed
Reforms that would have provided more funding to homeless utilizers of Medi-Cal health services — and tapped more federal dollars in the process — have been put on indefinite hold. Roughly $500 million approved in last year’s budget for things like mixed-income housing developments and new housing near transit was clawed back before it could be tapped by developers and cities scrambling to make projects “pencil out.” And the more ambitious plans, like the new system for delivering state homelessness dollars via “regional coordinators,” or imposing a state mandate to force local governments to make progress on their homeless populations (a plan Newsom never really embraced), have been ditched for now.
What’s left, now that we’re broke
The $750 million from the state for more general homelessness funding has been replaced by $750 million from the federal government for a specific purpose: buying some of the 15,000 hotel rooms the state has procured to provide emergency pandemic housing for the unhoused. Right now more than 7,000 of those rooms have been occupied, although the state does not track how many of those occupants are there for temporary quarantines as opposed to longer stays. The clock is ticking on the hotel purchases: The state has to make them by the end of the year or it loses the federal money.
With the federal funding restricted to acquiring and converting hotels to more permanent housing, Newsom is hoping counties and cities can fund homeless services like social workers and counselors with more than a billion in other federal pandemic supports, some homelessness specific and others for general coronavirus response. So far finding available hotels and motels for temporary homeless housing has proved less of a hurdle than staffing the hotels with appropriate health and safety net workers.
Finally, Newsom is keeping the $500 million in tax credits for low-income housing he proposed in January. Perhaps even more auspicious for low-income housing advocates, the vast majority of housing programs aren’t subject to $15 billion in “trigger cuts” Newsom warned would happen if more federal funding for states and local governments did not materialize.
What was conspicuously absent
Newsom’s pandemic-revised budget contains no new plan to help California renters and landlords beset by missed rent payments, a “looming crisis” for the state’s cash-strapped tenants. While the governor wants to push a $330 million windfall from a Great Recession-era lawsuit settlement to mortgage relief and legal aid clinics, that money is prohibited from being spent on rental assistance. Newsom administration officials have touted the rent relief package in House Speaker Nancy Pelosi’s most recent stimulus proposal, which would require signoff by both Senate Republicans and President Donald Trump.
What happens next
While Newsom’s housing and homelessness budget wasn’t as brutal as some were expecting, Democratic lawmakers and advocacy groups will still be fighting tooth and nail for additional funding they believe is necessary to ensure the governor delivers on pre-pandemic rhetoric.
At the top of the homelessness debate will be requests for billions in ongoing funds — money local governments and service providers can bank on every year to build shelters, operate converted motel rooms, and build permanent housing. Santiago’s proposal for $2 billion a year in new state homelessness funding does not identify a new revenue source (read: tax increase), meaning lawmakers would have to find $2 billion in cuts elsewhere. Another proposal from Sen. Jim Beall, Democrat from San Jose, similarly proposes roughly $2 billion per year for the next four years for homelessness and low-income housing development without specifying a new source of dollars.
Assemblyman David Chiu, Democrat from San Francisco, hopes his plan to eliminate the mortgage interest deduction on vacation homes to raise hundreds of millions in homelessness dollars will finally get through. His proposal has failed in past years.
“In this crisis we should be addressing the suffering on our streets rather than the tax breaks of the wealthy few who have vacation homes,” said Chiu.
Beyond the tug-of-war on homelessness dollars, lawmakers and Newsom will have to decide whether the state can afford a major rent forgiveness program, and if so how it should be structured.
State Senate Democratic leaders unveiled a plan they estimate would cost $300 million to $500 million per year that would allow renters to pay back missed rents over the course of decade, while compensating landlords with transferable tax credits. A separate landlord supported proposal would create a state program that would pay for 80% of missed rent payments.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
How California Community College Foundations Are Trying to Help Students
ByMikhail Zinshteyn, CalMatters
 In the third week of April, Shannon Hill approved the donation of some $35,000 in emergency aid to 40 students at Cuesta College in San Luis Obispo.
In the third week of April, Shannon Hill approved the donation of some $35,000 in emergency aid to 40 students at Cuesta College in San Luis Obispo.Hill, the executive director of the Cuesta College Foundation, the nonprofit arm of the community college, said that in a normal school year the foundation doles out $90,000 to $100,000 in aid. But given the economic toll the pandemic has taken on students, especially the many community college students who work part-time, the foundation is aiming to distribute closer to $250,000 this year.
It’s joining other local community college foundations that have been raising money or redirecting existing funds to help plug the gap that remains after state and federal aid.
At Cuesta, that means prioritizing undocumented students and others who were barred from receiving a portion of the federal stimulus money colleges and universities are set to receive through the federal CARES Act for pandemic relief that Congress approved in March. The stimulus dedicated $14 billion to higher education in the U.S. Of that, California’s higher-education sector is supposed to get at least $1.7 billion.
(Image: A student walks back to her car after picking up eggs, milk, produce and dried goods from the weekly drive-thru food pantry at Santa Monica College. Photo by Mikhail Zinshteyn for CalMatters)
“We do anticipate that more of our emergency grants will likely go to students who are not getting the CARES money, because we’ll be helping to fill that gap for our students,” Hill said in an interview late April, whose foundation is giving out grants of $1,000 to students and another $500 for students needing a second installment.
Money with strings
The country’s higher-education community cried foul when the U.S. Department of Education said in late April that the roughly $6.3 billion meant for direct student aid was off-limits to certain students, such as those who had defaulted on past federal loans, had below a C average, have certain drug convictions and are undocumented. One estimate is that there are 454,000 undocumented college students in the U.S., and a fifth live in California.
Democrats in the House and Senate wrote separate letters to Education Secretary Betsy DeVos saying that restrictions imposed by her department went against the spirit of the legislation.
And all that federal money isn’t enough to replenish the college budgets hampered by the pandemic or the aid students need. The Legislative Analyst’s Office warned in an April report that “initial data suggest that the federal relief funding provided under the CARES Act likely will be insufficient to address the full effects of the outbreak.”
Local philanthropy can help to close the gap. The vast majority of California community colleges have an associated foundation, like the one at Cuesta. Several foundation directors say they’re using their available dollars to support undocumented students, along with other students in need. The faucet of foundation cash turned on just as destabilization wrought by the COVID-19 pandemic became more apparent. The foundations responded to a wide range of student needs, such as food distribution, laptops or other mobile learning tools and emergency grants to cover rent. These efforts indirectly support students who wouldn’t qualify for CARES Act funding, foundation heads say.
“We have many, many students who would not receive any support from the CARES Act but will receive our scholarship funds,” said Lizzy Moore, president of the Santa Monica College Foundation. It raised $780,000 in scholarships to mete out to students, a banner year, Moore said.
The foundation also partnered with Los Angeles-based meal-delivery company EveryTable to send seven free meals weekly to 1,000 students, which works out to $44 spent per student a week, Moore said. By late April, she had raised $1.25 million in five weeks for the meal program, enough to keep it running through early September while feeding 1,500 students. It’s a service the foundation created toward the end of March after realizing students who relied on the college’s food pantries would be cut off from food as shelter-in-place orders closed campuses and pushed college instruction online. Anywhere from 100 to 200 students used the school’s pantries before the pandemic. Students are eligible for the meal-delivery program if they’re referred to the program by faculty or staff. In a nod to safeguard student privacy, recipients of the meal program don’t have to put down their actual names to receive the meals, Moore said. They could also request to send the meals to another address and pick up the shipment there.
Food for thought
The foundation also began running a weekly drive-thru food pantry to help students through the pandemic. On Wednesday, the pantry fed 289 students, who received a bag of fresh produce and shelf-stable food along with 18 eggs and milk. For eligibility, students just need to show they’re currently enrolled at the college.
“I don’t have to … risk to go out and buy food and second of all I don’t even have that money, so getting the food from school has been a blessing for me and my child,” said a student of the college who’s undocumented and requested anonymity. Through the foundation, she’s received the meal delivery plan and food from the pantry. The food alone saves her $150 to $200 a month, she said.
The immigrant from Cameroon works part-time as a homecare assistant. It’s just enough to cover her rent, but her priority is attending school full-time. Between her own school work, classes and assisting her daughter with her own lessons, “it’s heavy,” she said. Sometimes she brings her laptop, provided by the college, to work. When a patient sleeps, she opens her computer to keep up with classes.
And though she’s ineligible for federal financial aid, California’s financial aid programs are open to undocumented student residents. Her tuition is waived and she receives several state grants, including about $3,000 a semester for being a student with a child and $649 for attending school full-time.
“I just have no words, to be honest,” she said. “I just feel like I’ve been surrounded with good people.”

International students gain from the foundation’s efforts as well. Skander Zmerli came from Tunisia and studies at the college, where he’s a member of the student government. He receives free meals through the foundation’s EveryTable program. The college, he said, is compensating for “the fact that the federal government isn’t giving any financial support to international students.”
College foundations are limited in how much of their assets can go directly to students’ emergency aid. Because donor money has to be spent how donors want, foundations don’t have as much flexibility to change money allocation on the fly. At Chaffey College Foundation, which supports the Inland Empire community college, 93 percent of the foundation’s funds are restricted to scholarships and program support, said its executive director, Lisa Nashua.
(Image: Bags of produce sit moments before Santa Monica College’s weekly drive-thru food pantry opens up to students. Photo by Mikhail Zinshteyn for CalMatters)
Almost all of the Foothill-De Anza Foundation’s $40 million in assets are restricted. Still, the foundation, which supports the Bay Area colleges Foothill College and De Anza College, freed up more around $350,000 in discretionary funds for the colleges to use in response to the pandemic, said Dennis Cima, executive director of the foundation. It’s using the money as a stop gap until federal CARES Act money reaches students and for students who wouldn’t be eligible for the federal relief anyway.
The foundation has about $1.25 million in discretionary funds remaining, but it won’t use it all this school year. Cima said the foundation needs to anticipate the emergency aid support of students in the next school, especially if the economy continues to slide and more workers unable to find jobs head to community college to acquire new skills and request extra financial help.
In past years the foundation spent $25,000 to $50,000 from its discretionary pot, typically paying for end-of-year college events, student scholarships, supporting abroad studies trips, food pantries and other expenses. With shelter-in-place orders, those activities are unlikely to happen soon anyway.
By spending more now, the foundation will have less on hand once it’s safe for students to head back to campus. Cima will attempt to fund-raise more to refill the discretionary pool, but drawing down the money now to address an unprecedented need is the foundation’s role. “I am comfortable allocating these discretionary funds knowing the immediate need that our colleges and students have,” Cima said.
Formula mismatch
California community colleges enroll nearly 60 percent of the state’s college students but will only receive a third of the main federal funding made available to the state’s institutions of higher learning, according to the April report by the Legislative Analyst’s Office. Nationally, community colleges received less funding per student than did all other types of colleges, including public universities and for-profit colleges, according to a report by The Century Foundation.
The reason for the mismatch is because the CARES Act counted the number of “full-time equivalent” students instead of the number of enrolled students, a formula which “absolutely disadvantaged community colleges where significant shares of students are part-time,” said Debbie Cochrane, executive vice president at The Institute for College Access & Success. “For community college students, it really adds insult to injury.”
Community college students often can’t afford to attend classes full-time and need to work as well. As a result, using course units to determine relief money has different real life impacts for part-time students. One way to visualize this, Cochrane said, is to imagine two part-time students who now need laptops at home because classes moved online In that scenario, the logic of full-time equivalency falls apart. “Two part-time students can’t share one laptop. Two part-time students need two laptops,” Cochrane said.
All funds on deck
Beyond foundations, community colleges could access state funds to support students facing financial emergencies, including ones ineligible for federal financial aid. A state law passed last year allows community colleges to tap into a nearly $500 million annual pot originally intended for student advising and other academic support to also be used for student emergency aid.
Because the state law went into effect this year, it’s unclear how many colleges are using the funds — the Student Equity and Achievement Program — for emergency aid purposes. Assemblyman David Chiu, a San Francisco Democrat and author of the law allowing the money to go to student emergency aid, said in a statement that the emergency aid dollars could offer relief where the federal government does not.
“I hope that emergency grants will be a useful tool to support our community college students at a time when so many are struggling,” said Chiu. “Given that Secretary DeVos is using the COVID-19 crisis to play politics at the expense of our undocumented students, state-based emergency grants may give us an opportunity to step in and help these students.”

Despite the dire state fiscal situation, there are still ongoing efforts to send more money to students most affected by the escalating recession. The state community college system and the agency that oversees the main financial aid program is asking Gov. Gavin Newsom to send $500 in the upcoming school year to 82,000 low-income students, including nearly 12,000 undocumented students.
(Image: Santa Monica College student Skander Zmerli. He benefits from the college foundation’s free meal program. Photo by Mikhail Zinshteyn for CalMatters)
The University of California and California State University pledged to use internal resources to offer emergency aid support for undocumented students. A UC spokesperson did note that “the aid an undocumented student receives will be equivalent to the amount that an equally needy student who qualifies for CARES Act funding would receive.” The dollars come from flexibility the state has been giving the UC since 2013 to provide financial aid to undocumented students. A spokesperson for the CSU said its emergency aid for undocumented students at individual campuses “could come from a variety of sources including institutional funds, privately raised dollars, and foundation grants,” among others.
Fundraising during the pandemic is hard, some community college foundation directors said. Not only are benefactors being asked to support multiple nonprofits, but the shelter-in-place orders undermine the interpersonal touch that’s useful in highlighting to a potential donor a college program in need of philanthropic support.
“It’s hard to have a relationship with somebody that you can’t bring on the campus, you can’t visit them, you can’t have them see a program in action,” said Cima.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
In Reversal, Sonoma County Sheriff Will Enforce County’s COVID-19 Health Order

Updated Tuesday, 10:15 a.m.
The Sonoma County Sheriff's Office says it will enforce county health orders, reversing an earlier decision to stop enforcing the county shelter-in-place rules.
The change was announced in a joint press release Monday from Board of Supervisors Chair Susan Gorin and Sheriff Mark Essick. It says the county will “convene a Sonoma County Economic Recovery Taskforce focused on shifting our County from a broad, stay-at-home model that is based on essential/non-essential activity, to a risk-based model that weighs all available data.”
Essick had advocated for a “less restrictive, risk-based system” to mitigate the spread of the coronavirus in a previous statement explaining his decision to stop enforcement of the health order.
County Health Officer Dr. Sundari Mase said Monday on a call with the media that the county has always used a risk-based approach and sees no difference.
Mase last week said an increase in local COVID-19 cases merited caution as the county moves through the phases of reopening at its own pace.
The joint release from Gorin and Essick indicates that the county and sheriff’s office have turned a new leaf, and will move forward together in unison.
“We look forward to working together to achieve transparent decision-making processes; data-driven directives; thoughtful enforcement; and collaborative, cross-sector leadership,” it reads.
Original story:
Beginning Monday, June 1, the Sonoma County Sheriff’s Department will not be enforcing the county’s COVID-19 health order.
Sheriff Mark Essick in a Facebook post last week attributed the decision to a lack of information and transparency from the county about why it has not moved to a “a less restrictive, risk based system” to mitigate the spread of the coronavirus.
“As your elected Sheriff, I can no longer in good conscience continue to enforce Sonoma County Public Health Orders, without explanation, that criminalize otherwise lawful business and personal behavior,” he wrote.
Sonoma County District Attorney Jill Ravitch said Essick’s decision is at odds with other local law enforcement agencies and adds to fear and confusion around the pandemic.
“Yes, it is difficult to enforce and at times may seem arbitrary,” she said. “That said, the Sheriff and I both know our role is not to make policy but to enforce the rules.”
Ravitch said the decision to file criminal charges lies ultimately with the District Attorney's Office.
Essick met with county officials on Friday, including Board of Supervisors Chair Susan Gorin, Supervisor Lynda Hopkins, Director of Public Health Barbie Robinson and Sonoma County Public Health Officer Dr. Sundari Mase, to discuss enforcement of the health order.
Essick said in another Facebook post that while the discussion was “positive and productive in addressing the Sheriff’s concerns,” his decision to stop enforcement still stands.
He said the Sheriff’s Office will continue to educate the community and collaborate with the county.
-
Indoor Restaurants Shut Down in 72% of California for Three Weeks
By Lauren Hepler, CalMatters
 Beaches and bars were just the beginning. California Gov. Gavin Newsom today ordered indoor portions of restaurants, entertainment centers, museums and other businesses in counties with growing coronavirus outbreaks to shut down for at least three weeks.
Beaches and bars were just the beginning. California Gov. Gavin Newsom today ordered indoor portions of restaurants, entertainment centers, museums and other businesses in counties with growing coronavirus outbreaks to shut down for at least three weeks.As the Fourth of July weekend approaches, the indoor facilities must close in 19 “watch list” counties that are home to 72% of the state’s population.
Under the state order, restaurants, wineries, tasting rooms, movie theaters, family entertainment centers, zoos, museums and card rooms in those counties must close indoor facilities. Bars in those counties must close all operations, and many state beach parking lots also will be shut down this weekend, Newsom said.
“We have specifically targeted our operations to close indoor operations,” Newsom said during a press briefing today. “This doesn’t mean restaurants shut down.”
The impacted counties are Contra Costa, Fresno, Glenn, Imperial, Kern, Kings, Los Angeles, Merced, Orange, Riverside, Sacramento, San Bernardino, San Joaquin, Santa Barbara, Santa Clara, Solano, Stanislaus, Tulare and Ventura.
(Image: A sign outside of the Stanford Theatre announced its temporary closure in downtown Palo Alto on March 4, 2020. Photo by Nhat V. Meyer, Bay Area News Group)
Counties are added to the watch list when they exceed metrics that indicate that they have rising numbers of infections and hospitalizations. All counties under the new restrictions had been on the state list for at least three days.
On Tuesday, the state recorded 5,898 new cases, and California’s positive test rate has surged to 6.4% in the last week, up from 4.4 in mid-June.
In addition to the new closures, Newsom said seven state agencies are convening new “strike teams” as part of stepped-up enforcement efforts for businesses operating in violation of health orders.
“When people just thumb their nose, turn their back and put your life at risk, put their workers’ lives at risk, that’s why we have rules,” Newsom said. Of individuals who wear face masks as mandated by the state, he said, “It’s a sign of someone who gives a damn.”
The announcements follow several days of warnings about more aggressive state action to curb record numbers of COVID-19 infections in the past week, which have pushed the state past 6,000 deaths and more than 23,000 cases. On Sunday, the governor began “toggling back” some local reopenings by ordering bars to close in seven counties, including Los Angeles, and recommending that others on a growing state watch list do the same.
Local governments around the state have responded with a patchwork of closures during what is usually the summer’s busiest weekend.
Many residents are confused by the patchwork. In Los Angeles County, beaches will be closed from Friday through Monday. Next door, in Orange County, which previously attracted the governor’s ire for beach crowding and has emerged as a hotbed for backlash against health officials, most beaches are open, including popular Huntington Beach and Newport Beach. However, the city of Laguna Beach cancelled July 4 fireworks and closed its beaches, albeit only for the holiday on Saturday. San Diego is so far keeping beaches open but has implemented some restrictions on parking and indoor structures at area parks.
The new order means that no indoor dining rooms are open in Southern California for the next three weeks except in San Diego County.
Testing is also an ongoing area of concern, after Newsom reported a drop to 87,000 COVID-19 tests on Tuesday from some 105,00 tests on both Sunday and Monday. The state is also “pausing” a multi-million dollar test expansion effort in under-served rural towns and inner-city neighborhoods, the Los Angeles Times reported Wednesday, due to the program’s high costs.
 The new closures illustrate growing geographic divides in the pandemic’s California toll. Hospitalization rates are growing quickly in southern counties, including Imperial, San Bernardino and Los Angeles, the latter of which now accounts for nearly half of all cases statewide. Rural Central Valley counties with limited health infrastructure, including King, Stanislaus and San Joaquin, are also among those with the highest per-capita hospitalization rates and suspected new cases, a CalMatters analysis of state data shows.
The new closures illustrate growing geographic divides in the pandemic’s California toll. Hospitalization rates are growing quickly in southern counties, including Imperial, San Bernardino and Los Angeles, the latter of which now accounts for nearly half of all cases statewide. Rural Central Valley counties with limited health infrastructure, including King, Stanislaus and San Joaquin, are also among those with the highest per-capita hospitalization rates and suspected new cases, a CalMatters analysis of state data shows. In Northern California, where hospitalizations are still rising but at a slower pace, beaches have largely reopened in Santa Cruz and Marin counties, so long as visitors keep their distance. Some jurisdictions have voluntarily slowed or “paused” reopening plans, including more densely populated San Francisco, Alameda and Sacramento counties. Bars in the state capital were also ordered closed on Monday, and of particular concern in the Bay Area is a spiraling outbreak at San Quentin State Prison, where more than 1,000 cases have overwhelmed the health system.
(Image: Cleverson Davis, a waiter at Palermo Italian Restaurant in San Jose, tends to customers on June 5, 2020. Outdoor parts of restaurants can remain open in the state’s 19 “watch list” counties. Photo by Dai Sugano, Bay Area News Group)
“None of this should surprise any of us,” Newsom said. “As we reopen our economy, as more people mix, we’re going to see an increase in spread.”
Before Newsom announced the new restrictions today, he also extended some programs to ease the harsh economic toll of the virus, though largely keeping with a strategy to leave it up to local officials to decide what to ultimately implement.
Among the new authorizations in the executive order signed Tuesday night are the option for local governments to halt evictions for renters impacted by the COVID-19 pandemic through Sept. 30 — a move that housing advocates say is necessary to prevent a wave of mass displacement in high-cost areas. The measure also extends remote marriage and drivers license options, waives some Medi-Cal eligibility reviews and lengthens the window for confirmation of some state appointees.
Some 16 million Californians — more than half of all adults in the state — have seen their income fall since shelter-in-place orders in mid-March, according to a Census Bureau survey last month, which has strained state safety-net programs for housing, food and unemployment benefits.
-
Is Now the Time to Bring Back Affirmative Action in California?
 By Ben Christopher, CalMatters
By Ben Christopher, CalMattersDepending on your viewpoint, now is either exactly the right time or precisely the wrong time to take up a proposed change to the state constitution that seems certain to reignite a heated debate about race and justice in California.
At issue: a measure pending in the Legislature that seeks to reinstate affirmative action policies jettisoned by California voters two decades ago.
For supporters, events of the past week— city streets across the country filled with peaceful protesters and then scattered window smashing, thefts from store shelves and a few incidents of violence — show just how necessary it is to aggressively advance racial equity by fiat.
(Image: California lawmakers are revisiting whether to restore affirmative action policies for public schools and universities, as well as state jobs and contracts. Image via iStock)
Recent headlines “are forcing us to recognize that we are not beyond race as a country or as a state,” said Audrey Dow, vice president of The Campaign for College Opportunity, a Los Angeles nonprofit that advocates for more expansive access to higher education in California. “We have not achieved the nirvana of being color blind. Race matters.”
Opponents include a politically organized contingent of Chinese American Californians and Ward Connerly, a former University of California Regent who campaigned to ban state affirmative action programs in the mid-1990s. They argue that allowing schools and state agencies to take race into account when making admission and hiring decisions is its own kind of injustice.
“God knows we’ve got enough things in this nation that Democrats and Republicans argue about,” he said. “Certainly there should be some value that we hold to be dear and not fight over, like whether all citizens should be treated equally.”
In 1996, just four years after the last time the National Guard was deployed to Los Angeles to put down unrest in response to police violence, California voters passed Proposition 209, a constitutional amendment to ban affirmative action at state institutions.
The measure prohibits California’s state colleges and universities from taking into account the race, ethnicity, gender or national origin of would-be students in the admissions process. It also prevents state agencies from using such criteria in its hiring decisions or when awarding contracts for goods and services.
The Legislature can’t undo Prop. 209 on its own. Democratic Assemblywoman Shirley Weber of San Diego introduced Assembly Constitutional Amendment 5— a measure that, if passed by two-thirds of both the Assembly and Senate, will go before the voters on the November ballot.
A repeal of Prop. 209 would not mandate that state schools and agencies adopt affirmative action programs. But it would allow them to create employment or admission programs that explicitly take the race, gender or national origin of an applicant into account.
For some moderates and even some conservatives in Sacramento, the fact that the measure will present the question to voters rather than providing an answer unilaterally has been a vital distinction. In the Public Employment and Retirement committee earlier this month, Republican Assemblyman Randy Voepel, not known as a moderate, voted to pass it out of committee.
Prop. 209, he noted, had been passed by voters one “biblical generation” ago.
“This has got to go before the people of California of this generation,” he said, noting he had not yet decided how he would vote if the proposed constitutional amendment comes before the entire Assembly.
That will have to happen soon. Legislators have until June 25 to pass all potential ballot measures through both chambers. Repealing the affirmative action ban would be a heavy political lift even if the state’s extended shelter-in-place order hadn’t shortened the legislative calendar. It’s also made the in-person schmoozing that whipping votes often requires nearly impossible.
“I can’t get in their face and whisper in their ear, ‘You know you need to help me,’” Weber told Voice of San Diego.
Earlier this year, Assembly Speaker Anthony Rendon refused to endorse the effort. Though he said he supports the eventual repeal of Prop. 209, “if we are going to get something on the ballot, get it passed in November, from a political standpoint, it almost seems too late,” he told CalMatters. And that was in January, before the pandemic.
But with Weber’s proposal set to go today before the Assembly Appropriations Committee, chaired by San Diego Assemblywoman Lorena Gonzalez, a co-author, Connerly unhappily thinks the odds are in the measure’s favor.
“I will not be surprised if it passes the committee, the Assembly, the Senate,” he said.
In 1998, the year Prop. 209’s affirmative action ban kicked in, admission rates for black and Latino students across the University of California system dropped 10 percentage points for black students and 7 percentage points for Latino students compared to the previous year, according to admissions data. The numbers were much larger at the most competitive schools within the system — UC Berkeley and UCLA. A study commissioned by the UC Office of the President estimated that the system-wide affirmative action program that was in effect prior to 1998 increased the number of Latino, black and Native American students systemwide by 12%.
“The universities never recovered from 209 in terms of access for students of color,” said Gary Orfield, co-director of the Civil Rights Project at UCLA’s Graduate School of Education. “And there hasn’t been much progress across the state in diversifying faculties.”
Latinos, for example, make up 6% of professors and lecturers across the UC system.
Supporters of affirmative action argue that “race blind” admission policies that select applicants based on purportedly objective metrics like SAT scores or recommendation letters only reenforce existing inequalities. Such systems award coveted enrollment slots or jobs to those who can afford expansive test prep courses or who live in rarified social circles, the argument goes. Trying to bridge those racial chasms indirectly by using non-racial criteria like where an applicant lives or their family’s household income is tantamount to “willful ignorance” of the underlying issue, said Vincent Pan, executive director of Chinese for Affirmative Action, a nonprofit headquartered in San Francisco’s Chinatown.
For example, he said, “if you want to support Asian-owned businesses that have been affected by COVID-related racism, we should just have a program that supports Asian-owned businesses that have been affected by COVID-related racism.”
This is not the first legislative broadside against Prop. 209. In 2013 former Sen. Ed Hernandez introduced a similar repeal, applying only to public schools. That passed the state Senate on a party-line vote, but then faced fierce opposition from a coalition led by Chinese American social justice organizations. Their argument: Affirmative action policies in higher education would discriminate against Asian American applicants.
After a massive call-in, letter writing and capital lobbying campaign from opponents, Assembly Democrats refused to even put the measure up for a vote.
“We would never support a policy that we believed would negatively impact our children,” Assemblymembers Ted Lieu, Carol Liu, and Leland Yee — all Democrats — wrote at the time. The Wall Street Journal’s conservative editorial board referred to the campaign as “California’s Asian Spring.”
Opponents of Weber’s ACA 5 are counting on another wave of public pushback.
Wenyuan Wu, administrative director for the Asian American Coalition for Education, a national nonprofit, said so far there has been significantly more coverage of the issue in California’s Chinese-language press than in English-language outlets. Advocates, she said, have been organizing on WeChat, the Chinese messaging and social media app.
Yukong Zhao, president of the coalition, is a Republican candidate for Congress in Florida.
The reason that Chinese American Californias are among the most vocal opponents is obvious, Wu said.
Under any affirmative action system, “when a particular group of students are deemed as overrepresented,” she said, ”they stand to lose, they stand to be hurt by these kinds of admission practices.”
“Granted, there are inequities and structural issues that are rooted in deeper causes like unequal K-12 public education and deeper socioeconomic disparities,” said Wu. “But I don’t think ACA 5 is the issue. And in this case, I think the medicine might be worse than the disease.”
A national survey of Asian Americans in 2016 found that a majority of respondents supported affirmative action programs “designed to increase the number of black and minority students on college campuses,” compared to 32% who did not. Of the six national origin groups surveyed — Indian, Chinese, Filipino, Japanese, Korean and Vietnamese — only a majority of Chinese-American respondents opposed the policy.
“We know that there is some intense mobilization in some parts of the Chinese community but we try hard to help explain that actually the Asian American community is quite diverse,” said Pan of Chinese for Affirmative Action. Pan is also the co-chair of Opportunity for All, an umbrella advocacy group pushing to repeal Prop. 209.
He said that much of the opposition to Hernandez’s bill in 2013 came from relatively new immigrants, many of whom, he said, were misinformed about what the bill would actually do in a “cynical attempt by oftentimes white conservatives to exploit those concerns and direct them against race-conscious and gender-conscious policies.”
For decades, the U.S. Supreme Court has upheld the constitutionality of affirmative action programs, but on increasingly narrow grounds. Specific race or gender quotas were ruled unconstitutional in 1978. But the court held that schools may consider race as one of many factors when evaluating an applicant.
“Considerable deference is owed to a university in defining those intangible characteristics, like student body diversity, that are central to its identity and educational mission,” Justice Anthony Kennedy wrote in a high-profile affirmative action case in 2016.
But Kennedy is no longer on the nation’s highest court, and the bench has swung decidedly to the right. Chief Justice John Roberts, the court’s ideological center and frequent swing vote, has in the past taken a dim view of racially explicit policy.
In a 2005 case brought against the Seattle School District’s desegregation plan, which took into account a student’s race in determining which high school they ought to attend, Roberts wrote that “the way to stop discrimination on the basis of race is to stop discriminating on the basis of race.”
The court is likely to take up the issue of affirmative action in higher education again soon.
Students for Fair Admissions, a nonprofit run by conservative litigant and activist Edward Blum, sued Harvard arguing that its race-conscious admission policy represents “intentional discrimination against Asian Americans.” That case is awaiting a decision by a federal appellate court, but both sides have vowed to take the fight to the Supreme Court.
Whatever the high court does, Pan said that repealing California’s ban on affirmative action is still worthwhile.
“The right thing to do is always the right thing to do,” he said. “The best way to address racism and sexism is to address racism and sexism.”
-
Kaiser Employees Receive Help With Child Care, Shelter and Extra Leave Under Union Agreement
 A union agreement with Kaiser Permanente will ease the burdens of about 80,000 health care workers on the frontlines of the COVID-19 pandemic.
A union agreement with Kaiser Permanente will ease the burdens of about 80,000 health care workers on the frontlines of the COVID-19 pandemic.Under the agreement, members of the Coalition of Kaiser Permanente Unions will receive assistance with child care and temporary shelter, and extra leave if they are tested for or diagnosed with COVID-19. The agreement applies to full-time, part-time and per-diem employees.
The agreement focuses on three key areas:
Child-care assistance: With schools closed, many health care employees are having difficulty finding affordable child care. Under the agreement, Kaiser employees who work 32 hours a week or more in a KP facility will be eligible for a grant of $300 per week to pay for child care for children 14 or younger (and disabled, dependent children). It can be used to pay for their own caregiver (as long as they are not a spouse or domestic partner) or to find child care outside of the home.
The stipend will last until May 31, 2020, and will be pro-rated for employees who work between 20 and 32 hours (including per-diem employees) with a minimum of $210 a week.
Temporary shelter: Kaiser will work with several hotel chains to provide alternative shelter for employees who:
- Test positive for COVID-19;
- Work a double shift;
- Work multiple 12-hour shifts;
- Have fewer than 8 hours between shifts; or
- Have a household member who either has COVID-19 or is in a CDC-defined vulnerable group.
Eligibility applies to all employees working at least 20 hours per week (including per-diem employees) at a KP facility between April 13 and May 31, 2020.
Eighty additional hours of leave for employees who test positive for COVID-19: Employees working at a KP facility more than 20 hours a week (including per-diem employees) who test positive for COVID-19 will receive up to 80 hours of administrative leave. This is above and beyond regularly accrued leave. Employees who are sent home from Kaiser and are awaiting a test result will also be covered.
“As healthcare workers in the middle of this pandemic, we know our duty is to our patients and the community, and we take that duty very seriously. But we can only give our best if we know our own lives and our families are protected as well,” said Juanita Kamhoot, who works in surgical services at Kaiser Sunnyside Medical Center in Clackamas, Oregon. “This agreement will make a real difference at a time when we need every healthcare worker on the job and focused on taking care of COVID-19 patients.”
-
KBBF Informe: Licencia Por Enfermedad Remunerada, Paid Sick Leave
Por Edgar Avila, KBBF RadioThis episode was produced by Edgar Avila, KBBF Radio This article is a summary of a KBBF informe special loosely translated by NorCal Public Media. Listen to the original version in Spanish below. Puedes escuchar este episodio en español abajo:Welcome to this episode of KBBF Informe. Today we talk about emergency sick leave. How can we encourage people to stay in their homes if they have COVID-19? While the economy opens quickly and more people are returning to work, COVID-19 infections continue to rise. It is more important than ever that workers can protect themselves and for employers to protect their employees. One way of protecting workers is for them to have the ability to stay at home if they have symptoms of COVID-19, if they know they might be affected, or if they are at high risk.This is especially important for Latinos in Sonoma County because they are disproportionately affected by the coronavirus. Latinos represent 75 percent of all of the COVID-10 infections and many are front-line workers. One analysis shows that Latinos represent 76 percent of essential employees in industries like foodservice, healthcare, construction, and agriculture. Because of this reason having sick leave is critical. All workers can take three days off from work in the case of any illness, not just COVID-19.In terms of the pandemic, the federal government passed a law called the ‘Families First Law’ that says that employees who work at companies that have fewer than 500 employees have the right to ten sick days of paid leave in situations that are related to COVID-19. This law is to last through the end of 2020. A supplemental order from Governor Gavin Newsom means that people who work in the food sector including food service, restaurants, supermarkets, and agriculture, have the right to two weeks of paid sick leave independent from the size of their company.We spoke with Mara Ventura, Executive Director of North Bay Jobs With Justice, about this topic.Avila
This article is a summary of a KBBF informe special loosely translated by NorCal Public Media. Listen to the original version in Spanish below. Puedes escuchar este episodio en español abajo:Welcome to this episode of KBBF Informe. Today we talk about emergency sick leave. How can we encourage people to stay in their homes if they have COVID-19? While the economy opens quickly and more people are returning to work, COVID-19 infections continue to rise. It is more important than ever that workers can protect themselves and for employers to protect their employees. One way of protecting workers is for them to have the ability to stay at home if they have symptoms of COVID-19, if they know they might be affected, or if they are at high risk.This is especially important for Latinos in Sonoma County because they are disproportionately affected by the coronavirus. Latinos represent 75 percent of all of the COVID-10 infections and many are front-line workers. One analysis shows that Latinos represent 76 percent of essential employees in industries like foodservice, healthcare, construction, and agriculture. Because of this reason having sick leave is critical. All workers can take three days off from work in the case of any illness, not just COVID-19.In terms of the pandemic, the federal government passed a law called the ‘Families First Law’ that says that employees who work at companies that have fewer than 500 employees have the right to ten sick days of paid leave in situations that are related to COVID-19. This law is to last through the end of 2020. A supplemental order from Governor Gavin Newsom means that people who work in the food sector including food service, restaurants, supermarkets, and agriculture, have the right to two weeks of paid sick leave independent from the size of their company.We spoke with Mara Ventura, Executive Director of North Bay Jobs With Justice, about this topic.Avila
Mara, What is paid sick leave?Ventura
Paid sick leave means that the employer has to continue to pay the employee’s salary if an employee is sick or is caring for or living with someone who is sick, or can’t find childcare due to COVID. A sick worker receives their full salary while they stay at home taking care of their health. If someone is caring for someone else in their family who may be sick or is caring for a child so that they cannot go to work, they have to pay them at least 75 percent of their salary. We call for employers to pay 100 percent, nevertheless, it means that the worker could stay in their house taking care of their health or their family member’s health and still be getting paid.Avila
And why are these laws so important?Ventura
Part of our ability to flatter the curve of COVID is to ensure that people are sheltered in place. Particularly people who have symptoms or are caring for someone with symptoms and this is a luxury that very few can afford.
If people are working and depend on their salary to pay the rent, the bills, and groceries we have to find a way to replace this salary while they stay home sick. So that they don’t leave for work and possibly expose other people.Avila
Then this is especially important for essential workers, right?Ventura
Yes, absolutely, our essential workers sometimes don’t have the luxury of stable housing, like many of us, and so they have a greater risk. We need to make sure the employers respect these laws and offer better pay through workplace policies. As we reopen, it’s really important that all employees understand that they have sick leave. Every employer that is trying to bring their employees back to a worksite should assure that everyone understands not just workplace safety protocols but also what to do should they or someone they live with show symptoms.
Avila
What are the current laws?Ventura
O.K., so there are three measures of paid sick leave in effect. I want to be really clear that in the State of California, everyone has the right to paid sick leave. Before the pandemic, anyone had the right to three days of paid sick leave under state law. This has been the law since 2015 and it also says that one has the right to one hour of paid sick leave for every 30 hours worked.So people who had been working since January 1st had sick leave before shelter in place in March. Because of this, everyone who was working had at least three days of sick leave and possibly more if their employer did not place limits on how much they could accumulate. What congress did at the end of March was say that if you work for an employer that has under 500 employees, you qualify for seven additional days. In other words, you have ten days of paid sick leave. These days can be used by the hour for up to 80 hours and distributed as one needs them. But there is a limit of two weeks for people that work less than forty hours per week.What Newsom said is that he doesn’t think these laws sufficiently support workers in the food sector. Because of this, he decided to give them 80 complete hours without it mattering if their employer had over 500 employees. Agricultural workers in the field, restaurant workers, and grocery store workers have the right to 80 hours regardless of the size of the business they work for. This is very important. Imagine, for example, in a supermarket there might be more than 500 employees. The owner of the business, let’s say Safeway, employs more than 500 people throughout the country. These workers would have been excluded from paid sick leave under congress's act, but not under California’s.This is also very important for agricultural workers in the field, who for the most part, do not know that they are entitled to a full ten days or 80 hours of paid sick leave.Avila
Who has the right to these benefits?Ventura
Everyone has the right to paid sick leave in the State of California but the amount of days depends upon where you work.Avila
And what about undocumented workers?Ventura
It’s really important for folks to know that your immigration status does not change the majority of your rights as a worker. Everyone has the right to their pay, everyone has the right to paid time off, everyone has the right to overtime pay, and everyone, without regard to their immigration status, has the right to present a claim for wage theft. If you aren’t being paid appropriately or if you are not given paid sick leave, you have the right to file a claim with the California Labor Commissioner's Office. One of their offices is here in Santa Rosa. North Bay Jobs for Justice or the Graton Day Labor Center can help people present these claims.Avila
And if you submit a complaint, they won’t ask about your immigration status?Ventura
No, not at all. They support a lot of migrant and undocumented workers. They work really hard to make sure that every worker who files a claim receives their money. This includes anyone who took sick days and wasn’t paid. It also includes anyone who was denied using their sick leave.Avila
Is it complicated to get your benefits?Ventura
There is no paperwork. There are two other important things that I’ll say. One is that your only responsibility as an employee is to notify your boss. This doesn’t have to be in writing, but we encourage people to do it in writing so that you have proof if it is necessary later. The second important thing to know is that legally your boss cannot deny you sick leave in any circumstance, including if they cannot find a worker to replace you. Your boss cannot deny you even if they do not have sufficient funds. They have to allow you to take your sick leave. They have to allow you to stay home and not work and they have to pay you for it.Avila
So how does one apply for these benefits?Ventura
Because it is a right you already have, you don’t have to apply, you only have to notify your boss as soon as possible, when you or a member of your family has symptoms and you should be staying home. Also when you take a COVID test, they will give you a paper with instructions that say you should quarantine. You should show this paper to your employer if it’s useful or if they ask for it. If your employer asks you for a note when you come back they will also provide that.Avila
Are these notes obligatory?Ventura
That’s a good question, most likely they are because they fall under the health ordinances of Sonoma County. I’m not sure, but I imagine that there is a lot of concern at this moment because people do not want to take this test as they are going to tell you that you can’t go to work.We want to let you know that they do this test so that we can understand where the virus is and if the people that you are around are at risk. If you are working and you are worried about missing work without pay, you can let your boss know that you have the right to paid sick leave and that they should pay you while you stay home. You can call a community organization, like Jobs With Justice if you need help. In whatever case, you should absolutely get tested.Avila
And what happens if your boss says no?Ventura
If your boss says no, they are violating federal laws and regulations. Please call one of the organizations as soon as possible. We will mention a few numbers at the end of this interview that you can call. If you need help in other languages, we can also help with that.Avila
And what happens when the health orders and the quarantine are over?VenturaThe California State law is permanent. We will always have that, but the Governor’s order that provides leave for food service workers and the Federal law will end at the end of the year. It will probably be renewed in 2021, but for now, we are covered until January first.Avila
And if I have a business, can I get help to pay my workers who are home sick?Ventura
If you own a business with less than 500 employees and you pay a worker for sick leave it is 100% deductible from your taxes. The federal government will return this money. I also want to add that I believe that Sonoma County and the larger cities like Santa Rosa and Petaluma should consider financial assistance for small businesses so that some of this money can be recuperated immediately. Jobs With Justice is supporting this initiative. We have spoken with some of our elected officials. We have spoken specifically with the Hispanic Chamber of Commerce to support this idea. We want to encourage business owners to speak with their elected officials to talk about why paid sick leave may be financially difficult and ask what they can do to cover a portion of that cost.Avila
Many thanks to Mara Ventura. If you have problems with wage theft or not being about to take sick leave, you can contact these organizations.North Bay Jobs With Justice: 707 293 2863
California Rural Legal Assistance: 707 528 9941
Legal Aid of Sonoma County: 707 542 1290This KBBF Informe program was produced with Support from John S. Knight Fellowship of Stanford University. -
Keeping The COVID Plague at Bay: How California Is Protecting Older Veterans
By Dan Morain Dr. Vito Imbasciani has been at war with viruses since he was 5.
Dr. Vito Imbasciani has been at war with viruses since he was 5.Growing up near the U.S. Military Academy at West Point in New York, he contracted polio in 1952 and couldn’t walk for two months. In medical school in Vermont 30 years later, he witnessed AIDS steal the lives of otherwise healthy gay men.
Now, Imbasciani, secretary of California’s Department of Veterans Affairs, and his staff are responsible for keeping the novel coronavirus away from the state’s eight veterans homes. California’s defenses are holding.
The explanation, many say, lies in CalVet’s intense preparation, quick response, attention to hygiene and leadership, starting with Imbasciani, a physician and retired colonel who not too many years ago could have been discharged from the military because he is gay.
“We created our own fortune,” Imbasciani said, looking to knock on wood.
Deaths are part of life in the state-run veterans homes. The homes are populated largely by frail men and women, some of them veterans of World War II and Korea, and many from the Vietnam War era. A quarter of the vets admitted to California’s homes in recent years had been living homeless.
(Image: U.S. Air Force Maj. Joseph Knothe, a B-2 Spirit pilot from the 394th Combat Training Squadron, greets a veteran from the Missouri Veterans’ Home at Whiteman Air Force Base, Mo., Aug. 26, 2016. U.S. Air Force photo by Senior Airman Joel Pfiester)
COVID-19 has hastened the end for scores of retired soldiers in veterans homes in other states: More than 70 veterans have died of the disease at a “soldiers’ home” in Massachusetts; more than 125 have died in New Jersey’s three homes; more than 60 residents of an Alabama veterans home tested positive, and eight have died.
The California Department of Veteran Affairs, by contrast, is holding the beastly infection at bay. In its eight homes, where 2,100 veterans reside, three residents have contracted the disease, and two have died of it, one in his 90s and one in his late 80s.
“It’s all hands on deck,” state Sen. Bob Archuleta, a Los Angeles-area Democrat who chairs the Senate Veterans Affairs Committee, said of CalVet’s response. “It goes back to the staff. We have people who care about their veterans, and they will go the extra mile.”
Like Archuleta, Imbasciani credits the work of the front-line staff of nurses, nursing assistants and doctors who provide direct care. But leadership matters, and Archuleta and others also point to Imbasciani.
CalVet’s leader is a 73-year-old urologic surgeon who speaks six languages and has a master’s degree in musicology and a doctorate in philosophy. The son of a World War II tail gunner and grandson of a World War I vet, Imbasciani served 27 years in the Army Medical Corps. He deployed to war zones four times before retiring as a colonel in 2014.
For most of those years, Imbasciani had to hide his personal life because of President Bill Clinton’s “don’t ask, don’t tell” policy that sought to keep LGBTQ service people serving in the closet.
That changed when President Barack Obama signed legislation repealing the policy in 2010. Two years later, Imbasciani introduced Obama at a fundraiser hosted by LGBTQ community leaders in Beverly Hills.
“The price of my service was to live a lie,” Imbasciani told the crowd of 600 when introducing the president, as quoted by The Washington Post. “But not anymore.”
Imbasciani was director of government relations at the Southern California Permanente Medical Group in September 2015 when Gov. Jerry Brown appointed him secretary of the California Department of Veterans Affairs. Gov. Gavin Newsom reappointed him in January, even as the novel coronavirus was starting its global spread.
Over the years, Imbasciani has tracked SARS (severe acute respiratory syndrome), Ebola and Zika, among other viral threats. In January, when scientists in China sequenced the DNA of a mysterious new coronavirus that had emerged in Wuhan, Imbasciani thought, “Here we go again.”
He assumed the virus would storm the West Coast, as did CalVet’s director of long-term care, Thomas Bucci. Based on the devastating events unfolding in Wuhan, they quickly recognized COVID-19 as a disease far worse than the flu.
Bucci, an Air Force veteran, spent 38 years as a health care administrator before going to work for the state in 2015. Knowing that older and immunosuppressed people are particularly vulnerable, Bucci said: “We had a big bull’s-eye on ourselves.”
By mid-February, a month before the World Health Organization declared COVID-19 to be a pandemic, Bucci was regularly communicating with directors of the eight homes about the threat, and, along with Imbasciani, implementing a 38-step plan.
The protocol began with the basics. Directors of each home updated their emergency operations plans. They ensured they had enough surgical and N95 masks, gloves and gowns for the staff, and even disposable dinnerware, to minimize the chance of spread.
As of Feb. 26, all visitors were directed to sanitize their hands before entry, and staff began disinfecting common surfaces every 30 minutes. On March 4, as the infection killed the first of dozens of residents at the Life Care Center in Kirkland, Washington, Imbasciani discussed the coming onslaught at an executive team meeting. And by March 15 — four days before Newsom issued the statewide stay-at-home order — all visitors were barred, with the exception of family members paying respects to veterans in hospice.
Now, all staffers have their temperatures taken when they arrive for work and are sent home if they show symptoms. At four of the homes, all workers are encouraged to take tests for the virus, and all residents are tested. At the other four, employees who have been exposed to a known or suspected COVID-19 case are being tested, as are any residents who show symptoms.
All staffers wear masks, as do residents when not in their rooms. Residents are required to social-distance, meaning no congregating closely for conversation or card games. Meals are delivered to residents’ rooms.
The Veterans Home of California-Yountville opened in Napa Valley in 1884. How it withstood the 1918-19 influenza pandemic is for the most part lost to history. A century later, however, not a single COVID-19 case has been recorded among its nearly 1,000 residents.
Muriel Zimmer, 85, a Korean War-era Air Force veteran, has been living at the Yountville home for nine years with her husband, Dick. He needs more care and lives in the skilled nursing section of the facility, limiting her ability to see him. They’re allowed only brief conversations, and from a safe distance.
“I miss him,” she said.
She also misses seeing friends in the dining hall. But she remembers rationing during World War II, and knows others have it much harder. She is able to walk across the Yountville grounds, with its sweeping views of the Napa vineyards below, and notices small things, like the monarch butterfly that flitted by the other day.
“I almost get teary-eyed when I think about the staff,” she said. “We are blessed.”
At the Redding Veterans Home in Shasta County, Michael Vancleemput, a Vietnam-era Army veteran, spoke by phone through a mask, as a worker walked past disinfecting surfaces. “They’re personally motivated to serve us. It’s not like they’re doing a job,” said Vancleemput, 79.
He has to socially distance from his friends, not that it’s a problem. He lived alone for years in the small town of McCloud at the base of Mount Shasta before moving to the veterans home five years ago. A ham radio operator, he said he keeps in touch with other members of the home’s amateur radio operators club.
“I would invite you to visit our institution,” Vancleemput said, then paused. “Not now.” No visitors allowed.
The bulwark that CalVet has erected against COVID-19 builds on a series of improvements. When Imbasciani and Bucci arrived, the state-run homes used paper records. Now, medical records are tracked electronically. Each home once operated independently. Now, they are part of a system with standardized procedures.
CalVet’s nurses, nursing assistants and physicians are state civil servants with union representation and paid sick leave. One nursing assistant might be responsible for six or eight residents. At a private nursing home, an aide more typically handles 10 or 12. CalVet also has staff physicians on-site every day.
For many years, the federal government, which rates nursing homes, gave CalVet’s homes dismal marks. Now, among the homes that have been rated, four have the highest designation of five stars, and one has four stars.
“It does show that when there is strong and visionary leadership, it can make a big difference,” said Charlene Harrington, an expert on nursing home care and professor emerita at the University of California-San Francisco.
In the military, superiors give what are known as challenge coins to soldiers as an attaboy. The coins have a hierarchy. One bestowed by a two-star general carries greater bragging rights than, say, one given by a one-star general.
Imbasciani’s challenge coin is one of his most prized possessions. It’s a little larger than a silver dollar and is stamped with the presidential seal and the name of the 44th president. Obama gave it to him, and no one outranks the commander in chief, Imbasciani noted.
At California’s eight veterans homes, the walls are holding, so far. But Imbasciani knows an asymptomatic carrier could cause a breach any day. He is, after all, someone who has been battling viruses since he was a boy. He can even imagine the epitaph on his tombstone:
“Here lies Vito. He hated viruses.”
This KHN story first published on California Healthline, a service of the California Health Care Foundation.
-
Lawmakers Want to Know: What’s Up With That Half-Billion-Dollar Mask Deal?
ByLaurel Rosenhall, CalMatters
 California lawmakers plan to probe why state officials wired half a billion dollars for masks to a medical supply company that had existed for just three days, and want to know what’s changed in the state’s vetting process since the deal collapsed.
California lawmakers plan to probe why state officials wired half a billion dollars for masks to a medical supply company that had existed for just three days, and want to know what’s changed in the state’s vetting process since the deal collapsed.“We really need to ensure that there are appropriate controls in place and that we are spending California’s tax dollars efficiently and responsibly,” said Assemblywoman Cottie Petrie-Norris, a Laguna Beach Democrat.
The accountability and administrative review committee she chairs plans to hold a hearing this month to examine the bizarre transaction that CalMatters revealed earlier this week in which California wired $456.9 million on March 26 to Blue Flame Medical LLC – then scrambled to get the money back hours later. The company was incorporated on March 23 by two Republican operatives, Mike Gula and John Thomas, with no track record in the medical supplies field.
(Image: California lawmakers are demanding details about the state's vetting of Blue Flame Medical and other sellers of supplies to combat the novel coronavirus. Photo by Anne Wernikoff for CalMatters)
Republican lawmakers also are seeking an audit of all the state’s spending on protective masks, including the rescinded payment to Blue Flame and a $1 billion contract the state subsequently reached with a Chinese company called BYD.
“We are concerned about the details of a rushed, half-billion contract to a company only days old and a price-per-mask contract with BYD that could be nearly 40% higher than what is available on the market,” nine GOP lawmakers wrote in a letter to the Legislature’s Democratic leaders Thursday.
“Rather than learning of these issues from the Administration… we are getting delayed and incomplete reports from news stories.”
The state decided to cancel the deal with Blue Flame for 100 million N95 masks after bankers involved in the wire transfer alerted California Treasurer Fiona Ma that they were suspicious of it, Ma told the Sacramento Bee. Ma declined an interview request from CalMatters.
The account she gave The Bee portrays a deal that was about to close until two bankers called her to raise alarms. One bank executive was not comfortable completing the transaction because the Blue Flame Medical account had been opened just the day before, according to The Bee’s report, and another banker involved in the wire transfer thought the transaction might be fraudulent and planned to call the FBI.
“That’s when I called the governor’s office and said, ‘this is fishy,’” Ma told The Bee. “‘We got the money back, but you need to vet these people better and go through the proper protocol.”
Newsom insisted Thursday that his administration has improved its vetting process since the Blue Flame deal fizzled in the initial weeks of California’s coronavirus crisis.
“We were in the Wild, Wild West period in the early part of this pandemic,” he said. “Those dollars were protected and protocols were put into place that are much more strengthened after that specific incident.”
Newsom’s director of Emergency Services said the vetting process now includes a team of experts in health, logistics and foreign commodities as well as federal emergency management and law enforcement officials. But he acknowledged that decision making during an emergency is rushed, and that state officials were deluged with offers from people purporting to have the coveted medical supplies.
“There were thousands and thousands of individuals and organizations reaching out to us that required all of these aspects to be vetted,” Mark Ghilarducci said.
“And through that vetting process we actually were only able to get through a small percentage of legitimate organizations and companies that could provide the commodities we needed.”
Because Newsom declared the pandemic an official emergency, the state has waived many of the normal rules for procuring supplies and services. Vendors can land lucrative contracts with the state without going through the usual bidding process.
One key lawmaker lauded Newsom’s handling of the pandemic and said he trusts the state’s leadership.
“There has been no pattern ever in this administration or these departments of recklessness that would make me want to suggest that there was anything improper,” said Sen. Bill Dodd, a Democrat from Napa, who chairs a committee overseeing disaster response.
It’s still not clear why Newsom administration officials decided to make the deal with Blue Flame in the first place, given how new the firm is to the medical supply business. The state’s Department of General Services, which placed the order with Blue Flame, did not respond to several inquiries from CalMatters over the last week and a half.
“I think it would be very productive both for the Legislature and also for the public at large to understand what happened,” said Assemblywoman Petrie-Norris.
At the upcoming hearing, she said she intends to ask Newsom’s aides: “What we have learned, what controls and protocols are now in place, are there still issues and gaps, and if so how are we working to close them?”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Legislators Vote to Close School Spending Loophole
ByRicardo Cano, CalMatters
 State lawmakers are one step closer to plugging a technical loophole that has allowed California school districts to divert funds intended for needy kids to other purposes.
State lawmakers are one step closer to plugging a technical loophole that has allowed California school districts to divert funds intended for needy kids to other purposes.A legislative panel unanimously advanced a proposal that would strengthen oversight of how the state’s school districts spend money designated for needy students, making it one of the few surviving bills as the coronavirus pandemic has upended the state’s education agenda.
Assembly 1835 by Democratic Assemblywoman Shirley Weber of San Diego stems from a years-long effort to bolster transparency of the state’s landmark 2013 school finance law, the Local Control Funding Formula.
Advocates of the proposal have long argued that the law, intended to close gaps in student achievement, has lacked the necessary teeth to ensure districts appropriately spend additional funding meant for disadvantaged students.
But the proposal encountered new opposition from a group of school officials who argued that school districts need as much flexibility as possible to navigate looming steep budget cuts induced by the coronavirus pandemic. Experts and state lawmakers have warned schools of potential cuts in state funding greater than those during the Great Recession that resulted in mass teacher layoffs and years of painful cuts for schools.
(Image: Assemblymember Shirley Weber advocated for the Local Control Funding Formula in 2013, and now wants to close a loophole in the system. Photo by Anne Wernikoff for CalMatters)
Weber and supporters of AB 1835 said at a Wednesday morning hearing at the Capitol that the budgetary landscape only adds urgency for passing the proposal. Schools with high percentages of disadvantaged students, they said, experienced the brunt of last decade’s cuts, and they stand to be in a similarly vulnerable position without the legislation.
Weber, who lobbied legislators to pass the Local Control Funding Formula seven years ago, said she empathized with schools’ financial concerns, but said that the proposed changes remain long overdue.
“Even in good times for the last seven years, these kids have not benefited from these dollars because we have not held the districts accountable for using the money as it should have been spent,” Weber said. “We could not afford to once again fail these kids. Even in this pandemic, they are suffering the most.”
Signed into law by Gov. Jerry Brown in 2013, the formula overhauled how school districts in California receive funding. It replaced a system that was criticized for being inflexible and imposing strings for how schools could spend money.
The Local Control Funding Formula, which remains popular among school officials and education advocates, gave districts greater control in determining school spending while giving extra funding to districts with higher concentrations of students who are English learners, economically disadvantaged or foster youth.
Under the new formula, each school district receives a flat, per-student base grant. Districts with higher proportions of needy students receive additional funds with the expectation that schools direct those dollars toward disadvantaged students.
But the November state audit found that the law hasn’t done enough to ensure that districts are appropriately spending that money. The state audit, which renewed the effort to boost the law’s transparency, highlighted that unspent supplemental and concentration funds lose their designation after one year, essentially allowing districts to use those rollover funds for across-the-board expenses, such as teacher pay.
Wednesday marked the first time the Assembly Education Committee gathered since Gov. Gavin Newsom issued statewide stay at home orders on March 19. The legislative panel took up only a fraction of the bills it had been slated to consider this session as legislators shift their focus toward a budgetary landscape significantly different than the one the governor presented earlier in the year.
Prior to the pandemic, the state was on rosy economic footing, boasting a $21 billion surplus with plans to invest a record $84 billion for K-12 schools and community colleges. A revised budget later this month is expected to show a completely different picture, and school officials have warned that programs and services across the board will likely be affected by cuts.
Jeff Vaca, chief governmental relations officer for the Riverside County Office of Education, told lawmakers Wednesday that the county’s districts were not planning to oppose the bill. But, with tough financial decisions on the horizon, “we regretfully must oppose the bill because we believe it will make it more difficult to achieve our pledge and mission.”
“We will do everything humanly possible to prioritize and preserve programs for disadvantaged and at-risk students, and to mitigate the loss of learning that the crisis has already caused,” Vaca said before lawmakers advanced the bill. “But it is a certainty that all programs and services will be significantly impacted by the forthcoming recession.”
AB 1835 is among a handful of education proposals that will advance this session. The Assembly Education Committee had been scheduled to hear more than 140 proposals this session, though the panel took up only 13 bills in its sole scheduled hearing before a May 29 deadline.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Looming State Budget Cuts Pose ‘Incredible Financial Challenges’ For Sonoma County Schools, Superintendent Says
 Sonoma County’s Superintendent of Schools says the state’s landmark budget shortfall brought on by the coronavirus pandemic will pose “incredible financial challenges” for local schools in the coming year.
Sonoma County’s Superintendent of Schools says the state’s landmark budget shortfall brought on by the coronavirus pandemic will pose “incredible financial challenges” for local schools in the coming year.Superintendent Steve Herrington’s remarks come a day after Gov. Gavin Newsom shared his revised budget proposal, which features significant cuts to California’s K-12 schools and community colleges.
Herrington said the county Office of Education and local school districts run many programs, including CTE, workforce development, teacher development and special education preschool initiatives, that could see significant cuts as a result of certain grants or funding categories being scaled back. He also noted that all school districts will see a 10 percent cut in the Local Control Funding Formula (LCFF) funding that makes up the bulk of their budgets.
“These cuts will pose tremendous challenges at a time when districts are already underfunded and being asked to undertake costly social distancing measures in the fall, while also contending with declining enrollment,” he said.
Herrington said he strongly supports the governor’s call for federal aid to compensate for the state’s $54 billion deficit caused by record job losses. The Heroes Act proposal unveiled by House Speaker Nancy Pelosi asks the federal government for nearly $1 trillion for local and state governments.
Herrington said the county will be working closely with school districts to balance budgets, provide core student services and ensure student and staff safety.
“While these challenges are considerable, I have confidence that local school leaders will do everything they can do to ensure that all students receive the best education possible in the year ahead,” he said. “Now more than ever, our public schools are a critical component of the fabric of our society. Until school campuses reopen, our workforce cannot return and the economy cannot begin to rebound.”
-
Los Cien Sonoma County Hosts Congressmen for Virtual Coronavirus Town Hall
Los Cien Sonoma County
 hosted a virtual Coronavirus Town Hall on Friday with Congressmen Mike Thompson and Jared Huffman, who outlined the economic and health challenges facing the region, and federal programs to address them.
hosted a virtual Coronavirus Town Hall on Friday with Congressmen Mike Thompson and Jared Huffman, who outlined the economic and health challenges facing the region, and federal programs to address them.More than 300 people were registered to attend the Latino leadership organization’s first online-only, interactive conversation, hosted on Zoom and streamed on Facebook Live.
Thompson, who represents California’s 5th Congressional District, and Huffman, who represents the 2nd District, shared details of the legislation passed by Congress to address the fallout of the COVID-19 pandemic — namely the CARES Act and the Families First Act.
You can watch the full conversation, moderated by Santa Rosa attorney Oscar Pardo, below:
-
More Sonoma County Businesses Given Green Light for Reopening
 Additional businesses can reopen in Sonoma County, including car washes, pet groomers and outdoor museums, under an amended shelter-in-place order that went into effect Friday.
Additional businesses can reopen in Sonoma County, including car washes, pet groomers and outdoor museums, under an amended shelter-in-place order that went into effect Friday.The local changes follow Gov. Gavin Newsom’s statewide announcement Tuesday that more businesses could operate with health safety modifications as the fight against COVID-19 continues.
Under the amended order, the following businesses are allowed to operate and people are permitted to leave home and travel to work in or patronize them:
- car washes
- pet groomers
- dog walking services
- residential and janitorial cleaning services
- outdoor museums
- open air galleries
- botanical gardens
- and other outdoor exhibition spaces
The amended order also allows people to go back to work if telecommuting is not possible, and allows childcare facilities to open to those outside the essential workforce, following strict health protocols.
The order specifically lists businesses that must remain closed, which are: outdoor restaurants, cafes, or bars, zoos, amusement parks, indoor gallery and museum spaces, and personal care services that have close customer contact, including hair salons, barbershops, nail salons, massage parlors, aestheticians and cosmetology, ear piercing salons and tattoo parlors.
All storefront and indoor mall access remains closed to the public, though curbside pick-up, delivery and shipping are allowed.
The Sonoma County Economic Development Board has a new website offering resources for businesses on how to safely and successfully reopen. Industry-specific guidance from the governor’s office on reopening can be found here.
Find updates on Sonoma County’s response to the coronavirus pandemic at socoemergency.org. -
New State Child Care Website Comes Up Short
ByElizabeth Aguilera, CalMatters
 Gov. Gavin Newsom promised that the state’s new child care website would give essential workers all the information they need to choose a provider for their kids.
Gov. Gavin Newsom promised that the state’s new child care website would give essential workers all the information they need to choose a provider for their kids.It isn’t quite working out that way.
The portal Newsom announced a week ago, based on state licensing data, lacks key information. In many instances, hours of operation and available spots are missing. The site doesn’t indicate whether providers accept subsidies or what they charge.
The number of complaints about a provider initially was listed, but the state removed that information within days of the portal’s debut. Citations also are absent. To find that crucial information, a user would need to locate and then click on the license number — which then links to the state’s main licensing database.
(Image: Amanda Simoni, owner of Heritage School of Discovery in Oakdale, laughs while students play in the school yard mud pit. A new California child care website aims to connect essential workers with available options. Photo by Anne Wernikoff for CalMatters)
Across California, 72% of child care is provided by licensed private businesses — large centers and small and large family home care sites, accounting for nearly 1 million child care slots. Of those, 35% have a state or federal contract, such as Head Start. The rest get paid directly by parents or via vouchers.
Newsom said the portal was created to help working parents track down child care during the COVID-19 pandemic. The state’s shelter-in-place order never required private child care and preschool centers to close, but many have shut down for safety reasons or falling enrollment. Relatives who may have provided care or been backup babysitters are now in isolation, and schools are out for the foreseeable future.
But the portal is not proving to be a one-stop shop, said Nina Buthee, executive director of EveryChild California, a statewide organization supporting early childhood education programs with 1,500 members.
“Any parent would still need to make quite a few phone calls and reach out to a number of different places,” Buthee said.
Instead, she called the new California child care website a “really good start for finding out where facilities are.”
The new portal allows a user to enter an address or zip code to see a map of nearby centers as well as a list of providers. From there a parent can choose a provider and access whatever information is available. The portal lists 41,000 sites and 464 new pop-up child care locations.
The state Department of Social Services already had a licensing database that is searchable, but it is more complex and doesn’t provide availability information.
“The purpose of the portal is to provide child care options that are convenient and reliable for their families located near their work, home or preferred location,” department spokesman Scott Murray said in an email.
About the missing information, Murray said the department is contacting providers regularly through an automated system to get updates regarding availability. If a center does not respond to text, email or phone calls the site indicates “availability unknown.”
Originally the new portal included the number of complaints a child care provider has received but the state removed that information within three days. Murray said that element was cut because the page has a link to the original licensing site, where users can explore complaints, citations and facility inspection reports.
Buthee said if the goal was to create the informative, user-friendly site that Newsom promised, it should include a list of recent citations and complaints with the date, reason and resolution. Or instead, the site should explicitly explain what parents can find if they follow the link to the licensing data.
Ironically, there is a more in-depth child care database in the works. In July, a long-awaited multi-million dollar website will launch that includes in-depth information and resources for families. This project was created in response to the requirements of a Child Care Development Block Grant the state received in 2014.
The website was fully funded in last year’s budget, according to Keisha Nzewi, director of public policy for the California Child Care Resource and Referral Network, which holds the contract and is building the site.
“It’s good to have something up,” said Nzewi about the state portal. “I wish people could see how beautiful and user friendly this site is going to be. I wish COVID had held off or we had enough money to do this sooner.”
For now, the referral network is working with the state to infuse the portal with some of the features from the new site, like a more robust database of providers and availability.
The current California child care website has disappointed some parents and providers alike.
“It’s really bad,” said San Francisco mom Maria Jandres. “That portal doesn’t give you any information. It doesn’t say where they are, how many spaces. For a new parent it has nothing. It leaves you more lost and with even more questions.”
Jandres said her 4-year-old son’s regular child care site closed in March, around the time her work as a Realtor and court translator was coming to a slow stop. She stayed home with him for three weeks before signing up as a food delivery driver for various apps. She now juggles his care with her partner when he is not working.
“We have to figure out our child care because we don’t have anyone else,” she said. “Without child care neither my partner or I would be able to survive.”
At the same time, she said she is afraid to send her child to a provider she doesn’t already know, even if there are slots for essential workers. She’d rather ask around in her community for a personal recommendation.
This comes as no surprise to preschool owner Amanda Simoni, who went from having 54 kids every day to the 10 she is taking care of now at Heritage School of Discovery in Oakdale. She said she has laid off half of her staff and hopes to bring them back as soon as more kids return.
Simoni said California’s new child care website “came too late and it does not give enough information.”
She reached out to her local nonprofit child care agency after perusing the site and finding her phone number was wrong. It also included three complaints against her program, all of which were three or more years old and had been resolved, she said.
Simoni said parents should have all the information, but it should be listed in a comprehensive way. As is, she said, the portal is “just not giving accurate information, it’s not giving parents the opportunity to make a good decision.”
For parents seeking child care sites that are much smaller than Heritage School, and are operated out of a provider’s home, this portal is going to require some additional hoops.
These so-called “small family homes,” where providers care for up to eight kids, are listed without the official name of the business, address or contact information. Department spokesman Murray said that the contact information is not listed for privacy reasons because these are individual homes. So in order to reach these providers, parents would have to call their local nonprofit referral agency that oversees child care.
Those extra steps could thwart a connection between a family and a small child care provider.
“They need to have as much of an advantage as anyone else,” Buthee said.
Child care advocates hope to resolve all of these concerns with the new site.
Eventually, any searches will direct web traffic to the new site, Nzewi said. She said she expects the need to find child care to continue to grow into the summer, as some centers reduce enrollment to meet social distancing guidelines — or close altogether.
“It’s going to become even more important for parents and providers,” she said. “Parents will have to seek out new care.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Newsom Moves to Slash School, Health Spending — But Asks Feds for a Rescue
ByLaurel Rosenhall andJackie Botts, CalMatters
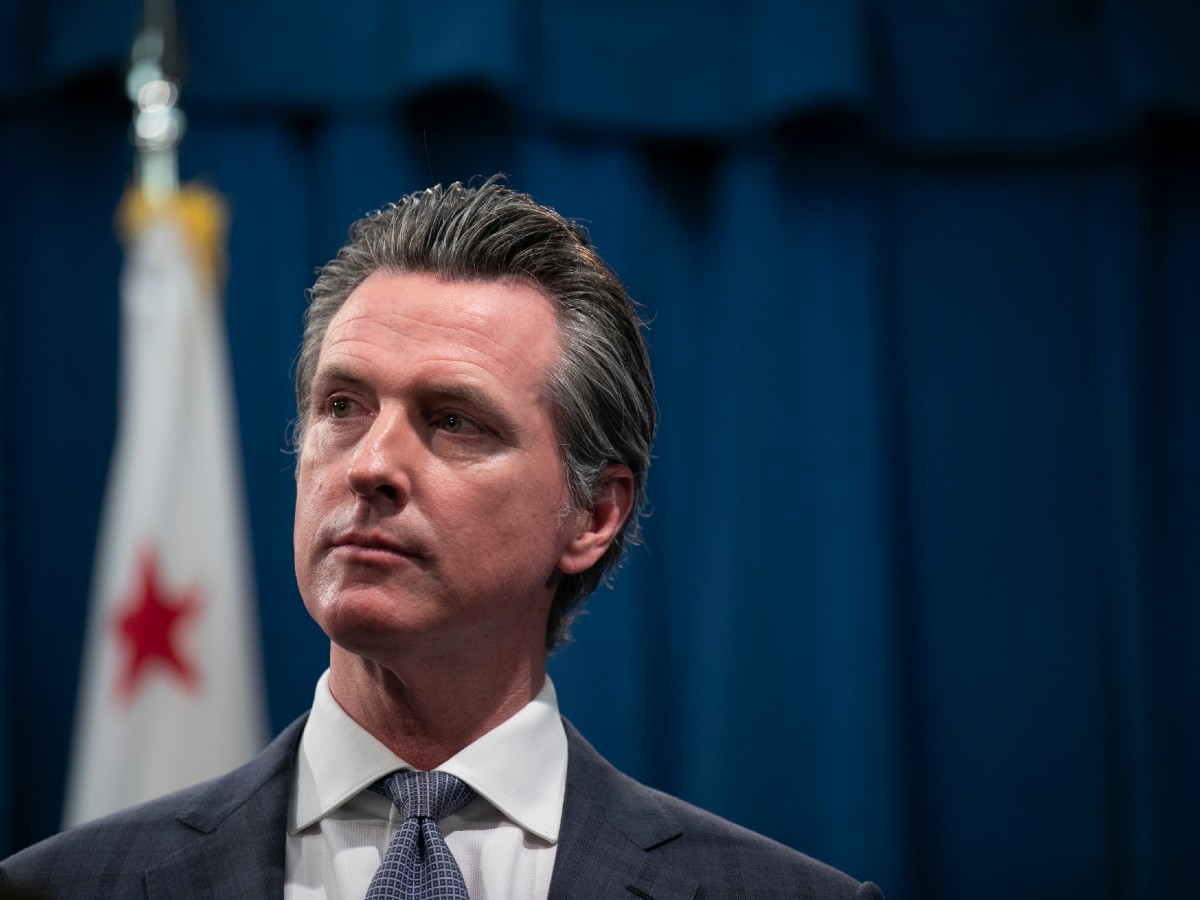 How does a liberal, blue-state governor take on the unappealing task of slashing the budget? By shifting a lot of the pressure to the federal government.
How does a liberal, blue-state governor take on the unappealing task of slashing the budget? By shifting a lot of the pressure to the federal government.In revising California’s budget down to $203 billion Thursday, Gov. Gavin Newsom charted a plan to fill a huge deficit by tying many cuts to additional federal aid. If the feds come through with $1 trillion for state and local governments that Newsom and other Democratic governors have requested, California would not reduce funding to schools, colleges, parks, child care, health care and other programs.
“The President of the United States, with a stroke of the pen, could provide support for Nancy Pelosi’s new HEROES Act and these cuts could be eliminated,” Newsom said, as he presented his proposal to close a $54 billion deficit brought on by record job losses during the coronavirus pandemic.
It’s a strategic, if risky, course as Newsom heads into a sprint of budget negotiations with state lawmakers over the next four weeks.
(Image: File photo by Anne Wernikoff for CalMatters)
On the one hand: Newsom’s proposed cuts will likely unleash an outpouring of advocacy from sympathetic constituencies including teachers, firefighters and police that could influence decisions in the nation’s capital. Newsom enjoys longstanding ties to House Speaker Nancy Pelosi, a fellow San Francisco Democrat whose father-in-law was business partners with Newsom’s grandfather. And despite feuds with Donald Trump that defined much of Newsom’s first year in office, he has developed a working relationship with the president. They have been publicly praising each other since the pandemic began.
On the other: GOP Senate leader Mitch McConnell has already rejected Pelosi’s latest aid package and previously said he wouldn’t support any “blue state bailouts.” Federal aid at the level Newsom would like — not to mention passage before cuts to the state budget would take effect on July 1 — is hardly a sure thing.
“We do need to have a Plan B,” said Assemblyman Phil Ting, a San Francisco Democrat who chairs the Assembly budget committee.
“I don’t think we should only rely on the federal government… If the federal money doesn’t come through, we should think about other options before we go to cuts.”
Ting’s counterpart in the state Senate sounded more optimistic that Congress would come through and that Newsom’s proposed cuts would not come to pass.
“The programs that he’s attached to the trigger hopefully will create a wonderful advocacy opportunity for beneficiaries of those programs to reach out to our congressional representatives to make sure that the state gets the resources they need so we don’t have to cut those areas,” said state Sen. Holly Mitchell, a Los Angeles Democrat.
Indeed, within hours of Newsom’s announcement, the California Teachers Association began asking Californians to call their members of Congress and urge passage of Pelosi’s aid package.
Lawmakers will now sift through Newsom’s proposal before they must pass a budget on June 15. GOP Sen. Jim Nielsen of Tehama quickly rejected Newsom’s approach, saying “relying on federal bailouts is not a budget solution.”
But Republicans make up just a quarter of the Legislature, not a large enough bloc to be influential in budget negotiations.
Most Democrats in the Legislature Thursday were elected since the last recession and now face their first bleak budget. Up until the coronavirus outbreak, California had enjoyed the longest economic recovery since the Great Recession. After raising taxes in 2012, the state managed its finances prudently in good years, paying off a $35 billion “wall of debt” from internal borrowing schemes and building up significant reserves — all of which helped improve the state’s credit rating.
Still, public employee pensions have since reported record losses. That has local officials fearful of service cuts, layoffs and even bankruptcy because state and local governments are obligated to contribute more — even when they have less. CalPERS, for example, shed $69 billion as the global financial market recoiled from the pandemic.
And former Gov. Jerry Brown, a doomsayer who paddled right of many legislative Democrats in seeking fiscal restraint throughout his second tenure, warned in his final state budget that the good times wouldn’t last forever.
“What’s out there is darkness, uncertainty, decline and recession,” Brown said in 2018. “So good luck, baby!”
The Newsom administration projects 24.5% unemployment, a 21% decline in new housing permits and a nearly 9% drop in California personal income for the fiscal year starting July 1. It’s a stark turnaround from January, when the governor laid out an ambitious agenda featuring a $5.6 billion surplus.
Newsom acknowledged all of that has disappeared “in a blink of an eye” as he walked back many of his January proposals. The governor dropped a plan to extend Medi-Cal health coverage to low-income undocumented seniors over 65 — a move that could cause friction with legislative Democrats hoping to support a community more vulnerable to the virus.
“Immigrants are the backbone of our state and have been serving as essential workers throughout this crisis,” Assemblywoman Lorena Gonzalez, a San Diego Democrat, said in a statement. “We are disappointed, but not surprised by the Governor’s actions to go backward on health for all.”
The crisis, however, may present opportunities for Newsom. He had proposed closing one prison in the next five years. Now he wants to close two prisons, one in 2021 and another in 2022. That will likely put him in conflict with the prison guards union that has traditionally wielded clout at the Capitol, but if Newsom is successful he would burnish his progressive bona fides in any future political campaign.
Broadly, the governor called for bridging the deficit by canceling non-essential spending, tapping reserves and borrowing. Among his proposals:
- Canceling $6.1 billion in program expansions and spending increases, including stopping a $2.4 billion extra payment to the California Public Employees’ Retirement System.
- Drawing down $16.2 billion from the state’s main rainy day fund over three years, and tapping a safety net reserve to offset increased costs in health and human services programs over the next two years.
- Moving $4.1 billion between accounts to help balance the budget, on paper at least.
- Temporarily suspending and capping tax credits used by businesses and wealthy taxpayers. Specifically, suspend net operating losses and limit to $5 million the amount a taxpayer can claim in credits in any given tax year. The move would generate $4.4 billion in 2020-21 to increase funding for schools and community colleges and maintain other core services.
California could look to its taxpayers in other ways as well, though it’s unclear whether voters will be in a mood to help. Labor and education groups are pushing a November ballot measure to overhaul Proposition 13, California’s landmark property tax cap, to help prevent steeper cuts to local governments and public schools. The Schools and Communities First campaign estimates the initiative could bring in $12 billion a year by raising commercial property taxes.
Newsom has not endorsed the proposal, which business interests vehemently oppose, but said he hasn’t ruled out asking voters for some kind of tax increase.
“We are considering other approaches, including other revenue strategies,” he said. “We will pursue conversations with the Legislature, with leaders all up and down the state and we hope we can help guide some consensus about what is most appropriate to put forward to the voters.”
In the meantime, about 26% of Newsom’s budget solutions rely on cuts he said would be eliminated if enough federal aid comes through.
“We are doing our best to help support people in need, but we now need the federal government to support not only the state of California, but other states across this country,” Newsom said. “If they do, if they meet this moment, we will be able to significantly reduce the stress and anxiety many are feeling.”
In other words: Washington, the ball’s in your court.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Newsom the Beneficent? California Governor Steps Into Pandemic Supply Vacuum
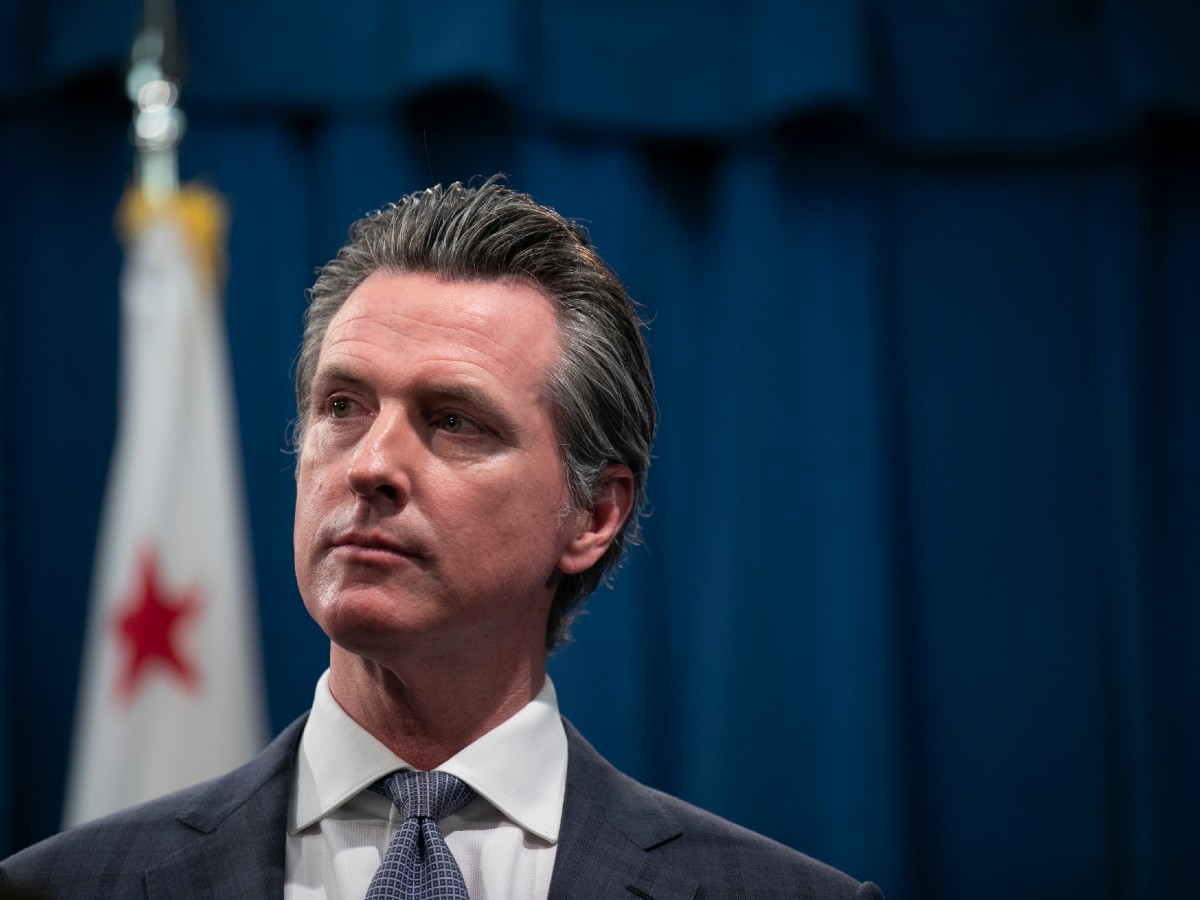
ByBen Christopher, CalMatters
California provides.
That’s the message that Gov. Gavin Newsom has been sending to the rest of the country over the last week. For those short on ventilators, the Golden State will share its mechanical bounty, sending hundreds to New York, New Jersey and Illinois, ferried by California’s uniformed National Guard.
For those who lack protective masks, California — as per an announcement he made on MSNBC’s Rachel Maddow show Tuesday night — will be amassing 200 million per month. Enough to meet the state’s needs. And maybe your state’s too.
“We need to coordinate and organize our nation-state status as we can, only in California with our procurement capacity that is quite literally second only to the United States,” the governor told reporters this afternoon. California would act as “a catalyst to increase supply” not only for the state’s health care workers, but for those in other states and perhaps other countries “across the globe.”
“That’s how we perceive our role.”
(Image: California Gov. Gavin Newsom / File photo by Anne Wernikoff for CalMatters)
Newsom’s offer to share California’s public health resources surely makes for good public health policy. No doubt, sharing extra health equipment during a pandemic is also good karma.
But it’s also good politics. Unsurprisingly Newsom, widely believed to harbor national political ambitions, refuses to characterize it in those terms.
“This is not political, this is not in any way, shape or form usurping or undermining, this is all in the spirit of all of us stepping into this moment and doing what we can,” he said in response to a question from CalMatters. “California is just uniquely resourced.”
In another crisis or under a different president, that’s a role one might expect of the White House. After spending the first weeks after the novel coronavirus made landfall in the United States downplaying its severity, President Donald Trump has since taken a rather hands-off approach when it comes to providing necessary supplies, coordinating purchases of protective equipment or using national emergency powers to force manufacturers to produce more of it.
Federalism or Darwinism?
“Try getting it yourselves,” the president advised state governors in a conference call in mid-March, a decentralized approach that former Maryland Gov. Martin O’Malley described as “a Darwinian approach to federalism.”
With the federal government receding, governors’ offices have attained a new kind of prominence, said California political analyst Sherry Bebitch Jeffe.
“We’re returning to the Articles of Confederation where the federal government is just there for war and printing money,” she said. “It’s the local and state governments — the governors — that are moving into the vacuum and creating the leadership and exercising the power in this crisis.”
For at least a decade, political focus and news coverage has been increasingly nationalized, with governorships, once a predictable stepping stone to the White House, fading from public view, she said. No longer.
On daytime television, “they are interrupting even the soap operas at noon to carry Newsom live,” she said. “I’ve never seen that!”
In that respect, Newsom still can’t compete with the star power of New York Gov. Andrew Cuomo. Chief executive of the state that has been hardest hit by the pandemic — and which is home to some of the country’s most prominent television and print news — Cuomo’s widely televised daily briefings have earned him a degree of national trust that seems to rival the president’s.
According to a Monmouth University poll conducted in the first week of April, 23% of respondents named Cuomo as the public official they trust most to deal with the pandemic. 20% put their trust in Trump. Only 3% named Newsom.
That may change now that Newsom is suggesting he could come to the rescue of some other states if California has spares from its equipment bounty. It’s yet another way that California’s governor has distinguished himself from his counterparts in other states. Newsom was the first to call for a statewide shelter-in-place order, issuing the edict days before Washington, New York and Louisiana and weeks before Arizona and Florida. In the weeks since, there are faint signs that California may escape the worst ravages of the virus — though it’s still too early to say whether Newsom and local leaders can take credit.
“Showing the world what makes our state great”
Another contrast in leadership styles: Amid a coronavirus outbreak aboard the Grand Princess cruise ship, Newsom coordinated with Oakland Mayor Libby Schaaf and the Trump administration to offload and quarantine the passengers in the Bay Area. He praised Schaaf and other local elected leaders for “showing the world what makes our state great — coming to the rescue of thousands of people trapped aboard this ship and helping tackle a national emergency.”
In Florida, where cruise ships loaded with sick passengers await disembarkation, Gov. Rob DeSantis said the state would only accept the Floridians.
In announcing his new plan this afternoon, Newsom evoked his Jesuit education.
“The Bible teaches us we are many parts, but one body,” he said. “Father Coz was my econ teacher at Santa Clara University and he began every single lecture by reminding us of our web of mutuality.”
Not everyone has applauded Newsom’s generosity. With hundreds of California ventilators lent out to other states in need, Riverside County Supervisor Kevin Jeffries, a former Republican legislator, told The Los Angeles Times that he worried whether regional hospitals would “be able to get the assistance that we’re going to need in a week or two weeks out.”
For now, plans to produce hundreds of millions of new masks and potentially provide them to other states remains a hypothetical.
Newsom said that a number of governors had welcomed his plan to mass-purchase equipment and share California’s excess “because they understand we are helping increase supply, we are not taking away a limited number of supplies.”
Newsom’s office has not yet responded to the question of which other states he was referring to.
Tara Lee, a spokesperson for Washington Democratic Gov. Jay Inslee, said in a statement that “Governor Newsom has expressed his hope that the California procurement system will soon be in a sufficiently strong position that they could share some of the opportunities with other states, and Gov. Inslee looks forward to discussing that.”
New Jersey Democratic Gov. Phil Murphy already has welcomed California’s ventilators:
-
Newsom: Cities Blocking Hotels for Homeless Will Be ‘Judged’ by History
ByMatt Levin, CalMatters
 As California scrambles to protect more than 150,000 homeless residents from contracting and spreading novel coronavirus, Gov. Gavin Newsom had some harsh words Saturday for cities he accused of blocking the conversion of hotels and motels for emergency housing.
As California scrambles to protect more than 150,000 homeless residents from contracting and spreading novel coronavirus, Gov. Gavin Newsom had some harsh words Saturday for cities he accused of blocking the conversion of hotels and motels for emergency housing. After touting the 10,974 vacant hotel rooms the state has acquired so far in a partnership with the federal government — roughly 4,200 of which are now occupied with homeless residents — Newsom charged some municipalities that have resisted the initiative with letting “not-in-my-backyard” politics interfere with a public health imperative.
(Image: A row of hotels and motels near Oakland airport on March 25. Gov. Gavin Newsom is encouraging cities to convert hotels into emergency housing to protect the homeless from COVID-19. Photo by Anne Wernikoff for CalMatters)
“I just want to encourage those cities that are blocking efforts like this to consider themselves in the context of others…to consider their actions in the context and annals of history,” said Newsom, speaking outside a Motel 6 in Silicon Valley that will be repurposed for the homeless. “They’ll judge themselves, not just be judged by others, by the extent they help the least among us.”
While Newsom declined to name specific problematic cities and praised others he said were eager to participate, his remarks suggest that the state’s unprecedented effort to convert hotel rooms to homeless housing has run up against a barrier beyond even the massive logistical hurdles of acquiring and staffing the hotels: political and legal challenges from local elected officials reluctant to allow COVID-19 positive and symptomatic homeless to be housed in their communities.
Resistance to the hotel initiative has surfaced most publicly in Southern California. The cities of Laguna Woods and Laguna Hills in Orange County, and Lawndale and Bell Gardens in Los Angeles County, have mounted legal challenges to hotels that inked emergency deals with county governments.
State, county and local governments across California have long fought over where homeless housing should be located, with few neighborhoods volunteering to devote land and resources to a population many residents associate with crime, mental illness and declining property values.
As the state prioritizes hotel rooms for the homeless who have tested positive for the virus or are symptomatic, a potent cocktail of fear is developing in some neighborhoods, say homelessness advocates.
“What is at stake right now takes this outside the realm of a conversation about NIMBYism,” said Shayla Myers, attorney for the Legal Aid Foundation of Los Angeles. “I think Gavin Newsom made the moral argument.”
A spokesman for the League of California Cities, which represents municipal interests in the Capitol, declined to comment on Newsom’s remarks.
Myers says that while she applauds Newsom’s rhetoric, homelessness advocates wish the governor would exercise more of the emergency powers granted to him during the pandemic to commandeer hotels or override zoning rules and other state and local laws cities use to mount legal challenges.
“The governor of the state of California has extraordinary authority in this moment of time to take concrete steps to address this emergency,” Myers said. “He is not using that authority to protect unhoused residents of this state.”
Beyond the admonishments to reluctant cities, Newsom on Saturday announced a partnership with Motel 6 that could include 5,000 more rooms in 47 motels across the state. While the state has negotiated a lease template with Motel 6, counties will ultimately determine whether to utilize the rooms.
Our most vulnerable unsheltered neighbors need protection from #COVID19.
— Office of the Governor of California (@CAgovernor) April 18, 2020
Today Governor @GavinNewsom announced a partnership with Motel 6 & secured up to 5k+ more rooms for Project Roomkey. #StayHomeSaveLives https://t.co/WQQ2trCN5BThe agreement with Motel 6 includes language that Newsom said will allow local governments to convert the sites into permanent homeless housing once the pandemic subsides.
Speaking with Newsom, San Jose Mayor Sam Liccardo said he hopes new rounds of federal funding will allow cash-strapped cities to avoid sending people who are homeless back to the streets. The Federal Emergency Management Agency has agreed to pay 75% of the cost of the motels during the pandemic, but funding after the emergency order is lifted is uncertain.
“We don’t want these rooms simply open for a few weeks or a few months; let’s give counties and cities the dollars they need to purchase motels so we can really aggressively address the homelessness crisis that will be here well beyond the time this pandemic passes,” Liccardo said.
In another sign that the pandemic is still not close to passing, Newsom reported that an additional 87 people had died as a result of COVID-19 in the past 24 hours, taking the state’s total death toll from the pandemic past 1,000, and that hospitalizations for the disease had ticked up 1.3%. The number being treated in intensive care units was little changed.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Ninth Person Dies From COVID-19 in Sonoma County
Adia White, NorCal Public MediaUpdated July 2, 2020Sonoma County's coronavirus death toll climbed to nine Wednesday night. The data was reported on the county's website socoemergency.org. This has been the deadliest week in the county with four people dying from the virus since Sunday, June 28.
State data shows that 22 residents have tested positive for coronavirus at Broadway Villa Post Acute. According to the Press Democrat, two of the recent deaths were residents at Broadway Villa. Other skilled nursing homes with coronavirus cases include Petaluma Post-Acute Rehab. According to state data, that facility has fewer than 11 cases though the data does not specify exactly how many.(Image: Capt. Mariana Lacuzong, critical care nurse, surgical intensive care/special care unit, 59th Surgical Inpatient Sq., administers patient medication through an IV in the Wilford Hall Medical Center ICU July 1. (U.S. Air Force Photo/SrA Josie Kemp)Counties across California have seen an increase in cases and fatalities, prompting the state Department of Public Health to order nineteen counties to shut down all indoor restaurants, wineries, movie theaters, zoos, and family entertainment centers. Indoor and outdoor bars were also ordered to shut down. Sonoma County is currently not on the state's watchlist, but Health Officer Dr. Sundari Mase said Wednesday that the county could soon meet those criteria and be ordered to close down some businesses. A case rate of over 100 cases per 100,000 residents could trigger mandatory restrictions and business closures from the state. Sonoma County currently has a case rate of 86.6 per 100,000 residents as of July 2, according to its website.On Wednesday Health Officer Dr. Sundari Mase also highlighted several other triggers that have sparked concern, including the number of available ICU beds. According to the county's website, there are 10 ICU beds available with 57 occupied.
The County of Sonoma's website reported 49 new coronavirus cases Tuesday and 44 new cases on Wednesday. There are now 1,229 total cases in the county. That number includes 620 people who have recovered from the virus.For more information on cases, hospitalizations and demographic data in Sonoma County visit socoemergency.org.This article will be updated as more information becomes available. -
Not An Option: Governor Orders Statewide Mask Use Amid Scattered Pushback
By Ana B. Ibarra, Cal Matters When hundreds gathered outside the state Capitol earlier this spring, demanding that Gov. Gavin Newsom reopen the state’s economy, some made clear they also had another message for him: You can’t make us wear a mask. One protester held a sign comparing face masks to dog muzzles, and many chanted and mingled without any type of face covering. But after weeks of mixed messaging and leaving the decision of implementing mask mandates up to counties, the state today said face coverings will be required after all.“Science shows that face coverings and masks work,” Newsom said in a statement. “They are critical to keeping those who are around you safe, keeping businesses open and restarting our economy.”Newsom, who has preached localism on many coronavirus-related matters, has often explained that a one-size-fits-all approach doesn’t work in a state with 40 million people. But as the state reopens and coronavirus cases and hospitalizations climb in some parts, a statewide mask order can perhaps make a difference in controlling further spread, some public health and county officials have said.Californians must now wear a face covering when interacting with other members of the public, and while in any indoor public space, as well as when in line to enter such spaces. These include pharmacies, a doctor’s office and the vet’s office. People must also wear a face covering while riding on public transportation, including a bus or a ride-share service, like Lyft or Uber.The state’s new rules don’t require face masks for children 2 and under and for people with a medical or developmental disability. People also don’t have to wear a mask during outdoor recreation, if they can keep six feet apart.(Image: Sinah Yovonie, 27, of Sacramento wears a mask while grocery shopping, but doesn’t think face coverings should be mandated. Ana B. Ibarra for CalMatters.)Disobeying California’s mandate could result in a misdemeanor and a fine, among other penalties, according to the California Department of Public Health. However, counties with their own mask mandates have learned that enforcement is challenging, and some have leaned toward “education” instead of penalties.Prior to the state’s rule, most Bay Area counties already had their own requirements. So did Los Angeles and San Diego. Some counties, including Riverside and San Bernardino, had temporary orders that were later lifted.Meanwhile, many other counties stuck to a “strongly encourage” approach.et even with the new statewide order, there is almost certain to be continued public resistance and polarization. Across the state and country, arguments over masks have prompted brawls, threats and other violent acts. In one extreme case, a security guard at a Michigan Dollar Store was shot and killed after a dispute with a customer who refused to wear one. But why?Psychologists and public health experts point to a variety of reasons: Some people don’t like being told what to do, while some are skeptical about the science or confused by the mixed messaging.For others, masks have become political.
When hundreds gathered outside the state Capitol earlier this spring, demanding that Gov. Gavin Newsom reopen the state’s economy, some made clear they also had another message for him: You can’t make us wear a mask. One protester held a sign comparing face masks to dog muzzles, and many chanted and mingled without any type of face covering. But after weeks of mixed messaging and leaving the decision of implementing mask mandates up to counties, the state today said face coverings will be required after all.“Science shows that face coverings and masks work,” Newsom said in a statement. “They are critical to keeping those who are around you safe, keeping businesses open and restarting our economy.”Newsom, who has preached localism on many coronavirus-related matters, has often explained that a one-size-fits-all approach doesn’t work in a state with 40 million people. But as the state reopens and coronavirus cases and hospitalizations climb in some parts, a statewide mask order can perhaps make a difference in controlling further spread, some public health and county officials have said.Californians must now wear a face covering when interacting with other members of the public, and while in any indoor public space, as well as when in line to enter such spaces. These include pharmacies, a doctor’s office and the vet’s office. People must also wear a face covering while riding on public transportation, including a bus or a ride-share service, like Lyft or Uber.The state’s new rules don’t require face masks for children 2 and under and for people with a medical or developmental disability. People also don’t have to wear a mask during outdoor recreation, if they can keep six feet apart.(Image: Sinah Yovonie, 27, of Sacramento wears a mask while grocery shopping, but doesn’t think face coverings should be mandated. Ana B. Ibarra for CalMatters.)Disobeying California’s mandate could result in a misdemeanor and a fine, among other penalties, according to the California Department of Public Health. However, counties with their own mask mandates have learned that enforcement is challenging, and some have leaned toward “education” instead of penalties.Prior to the state’s rule, most Bay Area counties already had their own requirements. So did Los Angeles and San Diego. Some counties, including Riverside and San Bernardino, had temporary orders that were later lifted.Meanwhile, many other counties stuck to a “strongly encourage” approach.et even with the new statewide order, there is almost certain to be continued public resistance and polarization. Across the state and country, arguments over masks have prompted brawls, threats and other violent acts. In one extreme case, a security guard at a Michigan Dollar Store was shot and killed after a dispute with a customer who refused to wear one. But why?Psychologists and public health experts point to a variety of reasons: Some people don’t like being told what to do, while some are skeptical about the science or confused by the mixed messaging.For others, masks have become political. Recently, Orange County became a battleground for face mask policy. This month, Dr. Nichole Quick resigned as the county health officer after receiving threats by people who opposed her mask mandate. Residents in opposition argued that the mask order was infringing on their rights to choose, while others said they weren’t persuaded by the science. Two days after Quick’s resignation, the county’s new acting health officer changed the county’s mask guidelines from “must” to “should.”
Recently, Orange County became a battleground for face mask policy. This month, Dr. Nichole Quick resigned as the county health officer after receiving threats by people who opposed her mask mandate. Residents in opposition argued that the mask order was infringing on their rights to choose, while others said they weren’t persuaded by the science. Two days after Quick’s resignation, the county’s new acting health officer changed the county’s mask guidelines from “must” to “should.”Orange County Supervisor Don Wagner said he never understood why the mandate was ordered in the first place, calling it “a real perplexing situation.”
“I asked why, I didn’t say no — I couldn’t — but I asked her to explain it to the people of Orange County and to the board of supervisors,” he said. “Instead of getting that explanation, she left her post.”
That said, Wagner said he does wear his face covering when out in public. He lives in Irvine and his city required it before the state did. He also said he believes there is a benefit to masks.
“I do think there is something to the argument that it can, especially if you can’t physically distance, help slow the spread,” Wagner said. “I wear it when I’m in a store and if I am going to be passing people.”
(A protester covers his face with an American flag during a reopen California demonstration on May 1, 2020, in Sacramento. Photo by Anne Wernikoff for CalMatters.)
The county’s clash of opinion was in full view this week when the Orange County Labor Confederation organized a press conference calling for a reinstatement of the mask order to protect essential workers. But the labor group was drowned out by anti-mask protestors, who showed up with a megaphone and signs that read “Show your smile” and “No masks.”
“Take your mask off, it’s not Halloween,” one woman shouted. “You look crazy!” yelled another.
One Placer County official said he will not be wearing a face covering, despite Newsom’s order.
“This has absolutely nothing to do with us reopening and it has 100% to do with the protests he allowed and encouraged,” Supervisor Kirk Uhler told CalMatters. He blames the jump in positive cases in his county on the Sacramento area protests following the police shooting death of George Floyd in Minneapolis.
But not all Californians who venture out without face coverings are ardent opponents.
In Sacramento, Wendy Valdez shopped at her local grocery store Wednesday, opting for no face covering. Her reasoning: it wasn’t required at the time. But if it were, she said, she’d wear it. “I just got my hair done and they required it, so I wore one,” she said.
Sinah Yovonie of Sacramento does wear a mask when grocery shopping. For him, it’s become a habit. But he doesn’t necessarily feel unsafe around those who aren’t wearing one, and he doesn’t like the idea of a mandate. “If you don’t want to spread it, you wear it, if you’re not bothered, you shouldn’t be forced.”
Dr. Susan Philip, a deputy health officer with the San Francisco Department of Public Health, said there is solid evidence that shows face coverings can help protect wearers from spreading the virus to others.
Sneezing, coughing and exhaling produces respiratory droplets, and a covering acts as a barrier that keeps these droplets from traveling.
San Francisco first issued its mask mandate in mid-April requiring coverings when entering an essential business or using public transportation. Officials then modified the order in late May to require that people wear coverings any time they left their homes.
“The thinking behind that is that as more of us start going out, we’re going to be around each other more and the face covering is one way to minimize the likelihood of transmission,” Philip said. “By having this in place for all of society we’re protecting each other.”
Because there are currently very few tools available to fight the spread of the virus, face coverings should be taken more seriously, some public health officials said even prior to the mandate.
Dr. Robert Wachter, professor and chair of the Department of Medicine at the University of California, San Francisco, said one of the reasons why mask wearing may have become so controversial is because of the messy, early messaging. For weeks after cases were first identified in the U.S., the CDC and state public health officials warned against face masks for the general public.
“In the very early days, people didn’t want to run out of masks, and that was not a ridiculous idea in March,” as shortages of protective equipment for health care workers became a top concern, he said. “But the messaging was too weak and inconsistent that some people took that to believe masks aren’t necessary.”
Matthew Normand, a psychology professor at the University of the Pacific, explained that wearing face coverings is like wearing safety gear in the workplace.
“You have to do some very intentional things to promote safety behavior, like wearing safety equipment,” he said. Workers will sometimes go without their gear because they’re uncomfortable but also because any consequence of not wearing it is often delayed or improbable, Normand said.
So if people don’t see the immediate danger, they may be less motivated to take safety precautions, he said.
If people aren’t too concerned with safety, then they might be more influenced by social aspects — like whether people around them are wearing masks and what those people are saying about face coverings, Normand said. That’s in part why face coverings have become political, he said.
Newsom doesn’t make a public appearance without his mask (even if ill-fitting at times). In contrast, President Donald Trump is rarely ever seen wearing one and has ridiculed his Democratic opponent, Joe Biden, for wearing one.
“It also is really helpful when we see people who are in positions of authority modeling appropriate behavior, and I think we know we don’t see that much right now,” Normand said.
“There’s probably no more important podium than the president’s podium, and if he had a mask on and people were standing six feet away from him consistently, that could have a very strong influence at least on the people that support him.”
-
Not Enough Patients: Health Clinics Struggle to Stay Open
By Erica Hellerstein, The Mercury News
 Community health clinics that serve some of the region’s most vulnerable residents are struggling with how to keep their doors open while patient visits plummet during the coronavirus shelter-in-place mandate.
Community health clinics that serve some of the region’s most vulnerable residents are struggling with how to keep their doors open while patient visits plummet during the coronavirus shelter-in-place mandate.Statewide, patient visits are down by roughly half across California’s network of community clinics and health centers, leading to tens of millions in lost revenue each week.
Many local health clinics that primarily serve low-income residents and rely on Medicaid reimbursements to make up a large portion of their income. So the dramatic reductions in patient visits threaten their ability to stay open and care for the kinds of patients who are at a heightened risk of contracting the virus.
Experts say the Bay Area, which has been in lockdown longer than anywhere else in the nation, has been particularly affected, with some already instituting furloughs or layoffs.
“The Bay Area clinics are hard-hit,’ says Carmela Castellano-Garcia, president and chief executive officer of the California Primary Care Association.
There are about 1,300 community clinics and health centers (CCHCs) across California serving more than 7 million patients annually — nearly one-sixth of the state’s population. Many provide care to residents particularly at-risk of contracting the virus or uniquely vulnerable to it. Community health centers serve roughly 1 in every 3 MediCal recipients, and in 2019 worked with 486,628 migrant workers and 246,268 homeless residents, according to CPCA.
With patient visits down, Castellano-Garcia says California’s community clinics are collectively losing about $90 million a week. Up to 77 health centers statewide may not be able to make payroll within 90 days if the current trends persist.
“It is not sustainable,” she says.
In the South Bay, patient visits at Gardner Health Services, which works in Santa Clara and San Mateo Counties, have dropped nearly 60%, says Chief Operating Officer Efrain Coria, prompting financial losses of about $1 million a month. Gardner has reduced its workforce by about 22%, Coria says, and laid off 135 staff members, though he emphasizes he hopes to re-hire many of them in the coming months when and if things calm down.
In the East Bay, La Clínica de La Raza, which serves about 90,000 patients annually in clinics throughout Contra Costa, Alameda and Solano Counties, has seen in-person visits drop about 30% since the start of the pandemic, says chief executive officer Jane Garcia, resulting in financial losses of about $3 million over the past month. About 300 employees have been furloughed.
However, La Clinica’s health centers have seen some gains since the state eased some restrictions for telehealth services, allowing patients to connect with health providers electronically. Those visits are also billable to Medicaid.
“If that option had not been authorized, it would have shut us down,” Garcia says. “And you would have seen [our patients] in emergency rooms and hospitals, or they wouldn’t have gone in at all.”
Marc Gannon, chief operating officer of Fremont’s Tri-City Health Center, which serves about 26,000 patients in Fremont, Hayward, Union City, Newark, and San Leandro — 37 % of whom are on MediCal or uninsured and the majority of whom live below 200% of the federal poverty level — says the organization changed its business model “essentially overnight” from in-person visits to telehealth appointments.
But the clinic is still suffering declines in revenue. In-patient visits have decreased by about 35% since the start of the pandemic and Gannon says they are considering reducing staffing to manage the financial hit.
“This is financially a very difficult time, there is no way of sugarcoating this,” says Gannon. “We are analyzing sustainability on a day to day basis.”
Amid the financial challenges, Tri-City health care workers are still trying to check in with patients by phone, providing resources from MediCal and other safety net services that they may be eligible for or with behavioral health services for people struggling with isolation and loneliness due to shelter-in-place orders. Last week, they reached 3,000 of the network’s 26,000 patients.
The federal government recently granted the nation’s federally funded community health centers a reprieve, awarding $1.32 billion to health centers nationwide. But many say that’s not enough to cover their losses. The $1.3 million the South Bay’s Gardner Health Services expects to receive, which is supposed to cover a 12-month period, would last between five and six weeks, Coria says.
Still, Bay Area community health centers want to make sure that people know their doors — virtually and physically — are still open to people who need care.
“Community health centers are adaptive, resilient, and have been around for a very long time,” says Gannon. “We are going to survive this.”
Erica Hellerstein is a journalist with the Mercury News. This article is part of The California Divide, a collaboration among newsrooms examining income inequity and economic survival in California.
-
Not If, But How: California Prepares for an All Vote-by-Mail Election in November
ByBen Christopher, CalMatters
 This coming November, every one of California’s more than 20 million registered voters may receive a ballot in the mail — whether they ask for one or not. In fact, many election administrators and advocates say it’s inevitable.
This coming November, every one of California’s more than 20 million registered voters may receive a ballot in the mail — whether they ask for one or not. In fact, many election administrators and advocates say it’s inevitable.“It’s not a question of ‘if,’ said Kim Alexander, the president of the California Voter Foundation. “But ‘how.’”
California is already ahead of the curve when it comes to voting from home. In the March primary election, 75% of voters got a ballot in their mailbox. But the exigencies of social distancing are putting pressure on state lawmakers to round that up to 100%, ensuring that every registered voter has the option to cast a ballot without having to physically crowd into a polling place.
A bill from Palo Alto Democratic Assemblyman Marc Berman would ensure just that. But with most state legislators sheltering in place until at least early May, all eyes are on the governor who, with an executive order, could make the upcoming election an all-mail affair.
Earlier this month, Joe Holland, president of the California Association of Clerks and Election Officials and top election official in Santa Barbara County, sent Gov. Gavin Newsom a letter requesting that he ink a new edict, declaring the November contest an “all-mail ballot election.”
Even if mass gatherings are permitted in November — something Newsom says is unlikely — county election officials say time is of the essence. Ballots have to be ordered, voter rolls assembled, polling places secured.
“The consensus for November 2020 is that California is going to go all vote-by-mail — and we should. We don’t want to have a Wisconsin debacle,” Holland said, referring to the April 7 presidential primary where some voters reported waiting in line for five hours. Since then at least three dozen voters and polling workers in Wisconsin have tested positive for COVID-19.
(Image: Sean Freese / Flickr)
The governor’s press office has not responded to a request for comment about prospects for a California all vote-by-mail election.
Even an “all-mail” election in California isn’t quite what it sounds like — it wouldn’t really be without a brick-and-mortar option. For those who need some extra help exercising their right to vote, state law requires counties to set up a certain number of in-person polling places.
Through Holland, the association also asked Newsom to grant them the authority to radically scale back that requirement. And therein lies the current rub.
Some advocates warn that an insufficient number of drop-off sites and vote centers could leave many voters — particularly those from underrepresented demographic groups — either unable to vote or stuck in long lines at the few remaining in-person locations.
“Waiving the state’s in-person voting standards will potentially disenfranchise tens, if not hundreds, of thousands of California voters,” union president Bob Schoonover, whose chapter of the Service Employees International Union represents tens of thousands of public sector workers across Southern California, wrote in a letter to Secretary of State Alex Padilla earlier this month.
Like so many debates of the COVID-era, it’s a disagreement that pits constitutional rights once thought to be non-negotiable against the prescriptions of public health.
“We’re trying to find the right balance of response that gives voters as much choice as possible, but also keeps them safe, and frankly, which is also implementable in the short number of months that the counties have to gear up,” said California Common Cause interim director Kathay Feng.
The coronavirus pandemic has injected new urgency into the national conversation about voting by mail, with some states now making it easier for voters to cast their ballots while self-isolating at home — and others not, and getting sued for it.
Despite evidence that making it easier to vote remotely does not benefit one party over another, the debate has taken on a partisan bent.
Weighing in earlier this month, President Trump urged Republicans to fight “very hard” against the expansion of vote-by-mail opportunities, claiming without evidence that such a system has “tremendous potential for voter fraud” and that “for whatever reason” such systems don’t “work out well for Republicans.”
The president’s views notwithstanding, recent polling has found strong majorities of Americans believe voters ought to be able to cast their ballots by mail without an excuse — though results are split on whether a majority of Republicans feel the same way.
But in California, there is little debate in policy-making circles about the merits of vote-by-mail elections.
Throughout April, Secretary of State Padilla — the administrator in chief of the state election system and, like Gov. Newsom, a Democrat — convened roughly 80 election officials, experts and advocates. They met, remotely, of course, in daily conference calls to game out how California might hold a statewide election during a full-blown pandemic.
Subgroups splintered off to hammer out every last logistical detail. Would registration deadlines be changed? How will each voter’s language preference be determined? Self-adhering envelopes that risk gumming up ballot-counting machines versus those sealed by pathogen-packed spit — how should counties decide?
Jonathan Stein, a program manager for the Asian Law Caucus’ voting rights program, was part of that task force. He said there was unanimity on at least one issue.
“There seemed to be almost universal agreement that we need to send every single voter a vote-by-mail ballot,” he said.
The question is, what other options will be available too?
Election rights advocates say in-person polling places offer a vital service to voters who don’t speak English, who experience some kind of disability, who don’t have a fixed address, who recently moved or who simply don’t feel comfortable with or do not understand the vote-by-mail process.
“There are a lot of communities that depend on polling places and polling centers,” said Mike Young, political director at the California League of Conservation Voters. In California, in-person voters skew poorer, younger and less white than the average voter.
An insufficient number of polling places could jeopardize public health even further, Young added. Like Holland, he pointed to Wisconsin as a cautionary tale. “People are anticipating that this is going to be an insanely high-turnout election.”
California voting rights advocates seem to have at least the tacit support of the state’s top election official.
“I think people who need or prefer an in-person option deserve it,” Padilla told KQED earlier this month. “And so we’re going to have to work really hard with counties to ensure we maintain as much in-person voting as we can.”
But county registrars argue that such requirements may put voters and poll workers at unnecessary risk.
“Quite frankly if we had an election tomorrow I wouldn’t be within a hundred feet of a polling place,” said Holland in Santa Barbara.
There are also practical questions about space and staffing, both of which are severely limited by the pandemic. Polling places are often hosted in schools, senior centers, and the garages of private homes — most of which are likely off the table now. The typical poll worker is a retiree, a cohort particularly at risk of severe COVID-19 complications.
Santa Barbara County is preparing to reduce the number of in-person locations from the 86 that were open in March to around five. Holland’s office may use the registrar’s three offices and then try to secure a handful of additional sites and the necessary poll workers.
“I don’t know if I can find three other facilities,” he said. “I have 15 staff and that’s when they’re here and healthy and right now three or four are out sick.”
Assemblyman Berman’s bill said his bill does not yet address in-person polling site requirements, but that the “first move shouldn’t be to weaken existing in-person voting requirements.” He urged state and county officials to be “creative” in finding locations and staff.
In the meantime, he said, some additional guidance from the governor could be helpful.
Newsom has already issued an executive order mandating that all voters in two upcoming special elections receive ballots in the mail. Though the order “encouraged” counties “to make in-person voting opportunities available,” they were given the freedom to do so “in a manner consistent with public health and safety.”
The two elections, a Senate race in Riverside County and a congressional contest north of Los Angeles, is showcasing how counties may differ in how they administer elections during a pandemic. In the congressional race, split between Los Angeles and Ventura counties, there will be at least a dozen locations where voters can drop off ballots in-person.
In Riverside County, home to the special Senate district, there will be only two physical drop-off points and no polling places or vote centers where voters can have their questions answered or their errors corrected.
“That’s a perfect illustration of what will happen if we give election officials full discretion,” said Stein.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Over a Million California Students Still Lack Access to Remote Learning
ByElizabeth Aguilera, CalMatters
 More than a month since officials closed schools due to the COVID-19 pandemic, California officials said a two-week blitz led by First Partner Jennifer Siebel Newsom has brought in 70,000 computers and other devices that will be distributed to needy students this week.
More than a month since officials closed schools due to the COVID-19 pandemic, California officials said a two-week blitz led by First Partner Jennifer Siebel Newsom has brought in 70,000 computers and other devices that will be distributed to needy students this week.Gov. Gavin Newsom has stressed the importance of distance learning and education multiple times during the past month — even talking about helping his own children with school work. Monday he focused attention on his administration’s efforts to secure donations from tech giants such as Google and Apple, garnering tens of thousands of computers and internet connections to children in need.
“For class to be in session, it is imperative that California addresses the inequities in access to computers, technology tools and connectivity to ensure that online learning can in fact reach all of California’s children,” Newsom said.
In addition, in Sacramento, the city is converting seven transit buses into super hotspots. Google is to begin establishing the first of 100,000 previously pledged hotspots during the first week of May. Already, Apple has distributed 10,000 IPads to 800 school districts and Google has given out 4,000 laptops.
Yet, even with all of the new devices going out in the coming weeks, it’s unclear if all of these efforts will really make a dent in the gap — highlighted by the pandemic — between those who have digital access and those who do not.
Siebel Newsom said one in five California children does not have connectivity or a device to access remote learning. Based on 2018-19 enrollment data, that means roughly 1.2 million children in California lack access.
“We all know that education is fundamental to opportunity and our mission will not end until every child has what they need to continue learning,” she said.
Previously, State Superintendent of Public Instruction Tony Thurmond said that the state is trying to get 150,000 devices in the hands of students who don’t have one.
This is especially critical for low-income students and students of color, Siebel Newsom said, referring to a recent study that showed 50% of low-income parents and 42% of parents of color “are worried about distance learning because they don’t have a personal device at home.”
Newsom also indicated the state will spend $30 million to connect more households that need it. Most of those funds, $25 million, will come from the California Teleconnect Fund and will be prioritized for rural, small and medium-sized districts.
The state Public Utilities Commission will also prioritize $5 million of the $30 million for computers for low-income communities.
The state Transportation Agency is teaming up with the city of Sacramento to convert the seven city buses into rolling super hotspots and get them going by May 1. These buses will provide connectivity within at least a 500-foot radius. Locations for the buses haven’t been announced. This is a pilot program that may be rolled out in other cities if it proves successful, according to Newsom’s office.
Since California began to track cases of coronavirus in the state, there have been 1,208 deaths, including 42 over the past weekend. Newsom said he will reveal a more detailed plan for opening up the state on Wednesday.
“We are not seeing the downward trend we need to see to provide more clarity on the roadmap to recovery,” he said.
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Pandemic Food Stamps Offer Up to $365 Per Child
By Jacqueline García, La Opinión
 Families with children who qualify for free or reduced-price meals at their schools — regardless of immigration status — may notice something in the mail to help them buy groceries.
Families with children who qualify for free or reduced-price meals at their schools — regardless of immigration status — may notice something in the mail to help them buy groceries. California is issuing one-time food stamps with credits of up to $365 per child to help qualifying families get through the coronavirus outbreak. The Pandemic-Electronic Benefit Transfer card, or P-EBT, from the Department of Social Services is an emergency disaster benefit that can be used to buy food and groceries, including online at Walmart and Amazon.
The first cards arrived last week for families receiving CalFresh, Medi-Cal or foster care benefits as a supplement to their EBT card. The second phase, which starts Friday, requires low-income families to apply at https://ca.p-ebt.org/.
(Image: California is sending pandemic food cards to qualifying students. In this file photo, Antionette Martinez and her son Caden, 5, who receive CalFresh, do their weekly grocery shop at FoodMaxx on July 26, 2019. Photo by Anne Wernikoff for CalMatters)
The deadline to apply is June 30.
The timing of this extra boost comes as many families struggle to provide nutritious meals for their children while schools are closed in response to the novel coronavirus.
Betzabe Castillo, who has a 9-year-old son at a public school in Stockton, California, was among the first to receive the P-EBT cards. She welcomes the help since her husband is the only one bringing in an income. Their rent is nearly $2,000 a month.
“It is very difficult because rent does not wait, the bills do not either,” Castillo said. “We are surviving day to day.”
Berenice Burgos, who has two children, ages 9 and 4, also received a P-EBT card last week. She wasn’t aware of the extra help but was grateful when it arrived in the mail.
“Right now I am not working and my husband, who is a mechanic, got his hours cut,” said Burgos, who lives in Concord, in Northern California. “It is very good help, especially for my children – to buy their milk, cereal and fruit because they want to eat all day.”
Much needed help while schools are closed
Jason Montiel, a spokesman for the social services department, said the state is offering additional assistance to children who are eligible for free or reduced price meals while school is closed.
The cards are distributed in two phases. The first batch of about 2 million went to families who enrolled in CalFresh, Medi-Cal, or foster care.
“For this phase, the beneficiaries do not have to do anything and the card will be mailed to them,” Montiel said.
The second phase requires residents to apply. The state projects an additional 1.8 million more children are eligible.
State officials say the card is available to eligible families regardless of a student’s immigration status or their parents’ status. It also doesn’t impact whether children are picking up grab-and-go meals from schools.
The food card isn’t considered a public charge by the Department of Homeland Security. However, the U.S. Citizenship and Immigration Services may consider several factors under its public charge test. Those who have questions should seek legal advice.
State officials also want recipients to be on alert for scams. Since the P-EBT cards began arriving in the mail, some recipients have received calls from people posing as social service representatives seeking personal information.
“The Department of Social Services will not contact clients or ask for personal information,” said Montiel. “We will not request a Social Security Number or any document that is shared with us.”
How do I learn more?
For more information about the P-EBT card visit:
Those interested should apply between May 22 and June 30:
If you have questions regarding public charge, visit: https://covid19.ca.gov/img/wp/listos_covid_19_immigrant_guidance_en_daf.pdf
Jacqueline García is a reporter with La Opinión. This article is part of The California Divide, a collaboration among newsrooms examining income inequity and economic survival in California.
-
Predicting a Pandemic’s Path: What Models Can and Can’t Do
ByBarbara Feder Ostrov, CalMatters
 Every day, while we’re all stuck at home, politicians and health officials and news anchors point to graphics showing the latest statistics on the coronavirus pandemic to indicate what might happen next, in your region and around the world.
Every day, while we’re all stuck at home, politicians and health officials and news anchors point to graphics showing the latest statistics on the coronavirus pandemic to indicate what might happen next, in your region and around the world. Underlying those visuals are disease forecasting models — complex mathematical algorithms that predict disease spread and severity based on different scenarios. Because they can help predict the effects of different interventions, including our social distancing, coronavirus pandemic models significantly influence how governments are responding.
It’s tempting to regard these models as oracles that can tell us precisely what to do and when to do it. Can they tell us when we should return to work, or when our kids can go back to school? Is Grandma safe in her nursing home or should she come home? When can businesses safely reopen?
As California’s COVID-19 caseload tops 30,000, state officials are using a model developed at Johns Hopkins University to aid in their planning. If you’ve watched Gov. Gavin Newsom’s daily briefings online, some of the charts shown are based on the model’s predictions.
But the models need to be fed reliable data, and some data is in short supply, especially without widespread U.S. testing for the novel coronavirus that causes COVID-19. We still don’t know how many people have been infected without symptoms, for example. Other inputs, such as incubation periods and death rates, change by the day as we learn more about this virus.
“What makes modeling especially challenging are the human factors. Individual behaviors, health care infrastructure and political response each can affect the outcome of an epidemic,” said Shweta Bansal, an associate professor of biology at Georgetown University who specializes in disease modeling. “I think of models as a call to action. They can tell us what happens if we don’t act and how we can prevent the most dire consequences.”
Here are five things you should know to make sense of infectious disease models:
Why are there so many COVID pandemic models — and why are they all so different?
There are different types of infectious disease models for different purposes. Each has limitations and each can be useful in its own way.
“SEIR” models, for example, involve equations based on the number of susceptible people (S) who can be infected, the number of people exposed (E), the number of people infected (I) and the number of people recovered(R). Agent-based models use massive computer power to simulate the actions of millions of hypothetical people to predict the spread of disease. Still other models examine a disease outbreak in one country and try to predict outcomes elsewhere in the world based on that data. Some models look at travel patterns in spreading disease, and still others assess how age, ethnicity and contributing illnesses may affect survival rates.
Epidemiologists say it helps to have more than one model in responding to disease outbreaks because they use different inputs. Combining results from multiple models can give a more nuanced picture of an outbreak’s trajectory.
“The fact that there are so many models is a healthy sign,” said Bansal. “It’s the same with weather forecasts that rely on multiple mathematical models. But unlike a weather forecast, with a disease forecast we have the ability to change the outcome.”
The White House has controversially used a model developed by the University of Washington’s Institute for Health Metrics and Evaluation, which some disease experts have criticized as being based on overly optimistic assumptions about the benefits of social distancing, among other statistical issues. The Imperial College London model, which predicted as many as 22 million U.S. deaths if no action was taken, also apparently prompted the Trump administration to issue tougher new social distancing guidelines.
What goes into making an epidemiological model for an infectious respiratory disease?California and some other states use an SEIR model developed by Johns Hopkins University epidemiologist Dr. Justin Lessler. This coronavirus pandemic model, according to the California Department of Public Health, takes into account assumptions about how long the disease takes to incubate, how long people are infectious, how many people each patient can infect, the fatality rate, how many people need hospitalization or intensive care, and importantly for hospital planning, how many people need ventilators because they can’t breathe on their own.
The model assumes that NPIs – “non-pharmaceutical interventions” such as social distancing – started in the state March 20. In fact, some counties ordered residents to shelter in place earlier, some later.
California also has been faring better on a daily basis than this model’s predictions had forecasted — only 4,892 cases were reported on April 16, compared to 12,119 cases projected for that date. Assembly members set aside time at a budget hearing Monday to question the Newsom administration about the model and seek more details about its assumptions.
Rodger Butler, a spokesman for the California Health and Human Services Agency, cautioned that “there is considerable uncertainty” in the model’s predictions because we still don’t know enough about how the virus behaves and, without widespread testing, how many people are infected. “We are continuously refining our model with researchers and local public health offices,” Butler said.
Which raises the next question:
What happens if you don’t have enough data, or the right data?
This is what keeps public health experts up at night.
Because testing has lagged so badly in the United States, “right now we don’t know how many people are infected,” said Karin Michels, professor and chair of the epidemiology department at UCLA’s School of Public Health. “The biggest unknown (for disease models) is the denominator. How many people out of the infected are actually dying or wind up in the ICU? We have no idea at this point.”
Epidemiologists want to know more about when people are no longer infectious. They hope to learn more about who, once infected, is most likely to need hospitalization or a ventilator, to prevent overwhelming hospitals. True fatality rates aren’t one-size-fits-all; they will differ by age, gender, underlying illness and access to health care, among other factors.
Epidemiologists also need to better understand how many people might have been infected but not show symptoms. New antibody tests now being rolled out can help answer that question, but not quickly, and some of these tests are proving inaccurate. Some public health experts say that preventable delays in widespread testing and a perceived chaotic federal response have prevented the kind of critical data gathering needed to get a handle on outbreaks in various regions of the country — and to provide the kind of intelligence needed before reopening the country.
What makes a model succeed in its predictions?
Disease modelers and mathematicians argue about this a lot. The quality of the data that goes into a disease model is important. The range of error in the model’s predictions are important, too. If early predictions of a model don’t measure up to reality, its later predictions may not as well.
The University of Washington’s coronavirus pandemic model, for example, which aimed to predict outbreaks based primarily on early data from China and later Europe, has had such a wide range of error in its predicted death rates that some epidemiologists have recommended that governments do not use it for planning. The model’s predictions of when cases will peak in various regions also have swung dramatically in different weeks — and rarely coincided with other models’ forecasts, prompting some experts’ concern about the model’s validity going forward. Some politicians are citing the model’s relatively optimistic forecasts as justification to open the country earlier than public health officials recommend.
The model’s developers say they are continually updating their model and have adjusted it to reflect regional differences in how daily death rates peak over time, and how social distancing policies vary by region.
Still, disease models are supposed to serve as a wake-up call prompting us to act. If our actions succeed in slowing infections and deaths, making the predictions inaccurate — that’s a good thing.
What do public health experts wish people understood about coronavirus pandemic models?
Disease models are not perfect, and they can adapt as new data becomes available. Models “can help us think through different scenarios, but they shouldn’t be used as crystal balls,” Bansal said. “If we believe that a model’s prediction of 100,000 deaths is what will happen if we don’t act, then we do everything we can to prevent those 100,000 deaths.”
Also: they’re better for predicting short-term needs and outcomes, Michels said, such as how many ventilators a hospital might need next month, rather than next year:
“I don’t think we can predict the fall yet. We only know the virus will still be around, so life will be complicated.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Private Colleges Brace for Downturn Amid Pandemic Fallout
ByFelicia Mello, CalMatters
 Nikolas Schumann was a community college student and budding painter when he first learned about the San Francisco Art Institute from a mentor. He visited the school, “absolutely loved” it, and decided to transfer there in 2018 after a large scholarship knocked his tuition from $46,000 per year down to $15,000.
Nikolas Schumann was a community college student and budding painter when he first learned about the San Francisco Art Institute from a mentor. He visited the school, “absolutely loved” it, and decided to transfer there in 2018 after a large scholarship knocked his tuition from $46,000 per year down to $15,000. “It just had so much history and was so diverse,” Schumann said. “They birth interesting and wild artists.”
But just a few months from graduation, Schumann’s plans are in limbo after the art institute, along with another Bay Area college, Notre Dame de Namur University, said last month they would not be enrolling any new students in the fall. Art institute officials cited the coronavirus outbreak as a factor in their decision.
The news from the two schools — one a Catholic university that was the first in California to admit women in 1868, the other a fine arts academy that counts photographer Annie Leibovitz among its alumni — highlights the financial challenges facing the state’s small private colleges as the pandemic imposes new costs and throws the admissions cycle into turmoil.
(Image: Painting major Nikolas Schumann picks up a canvas from the closed Chestnut Street campus of San Francisco Art Institute. Schumann says he will likely transfer to California College of the Arts next year to finish his degree. Photo by Anne Wernikoff for CalMatters)
Unlike public universities like the University of California system, private colleges cannot count on state tax dollars to keep them afloat. Many of their most attractive selling points, from charming campuses to face time with professors, no longer apply in a world where instruction has moved online. With families less willing and able to pay tuition that can reach $50,000 per year for what some have dubbed ‘Zoom University,’ the pandemic has raised fears that a growing number of independent colleges could scale back, merge or even shut down.
“Most schools do not have large endowments that could provide the rainy day fund that we need right now,” said Kristen Soares, executive director of the Association of Independent California Colleges and Universities, which represents private, non-profit colleges. “If this goes into the fall, it could be very devastating.”
Most at risk, experts say: less-selective residential colleges that are not well-known outside their local area. The Midwest and Northeast have seen a wave of closures among such schools. California, with its larger population of college-ready high school graduates, hasn’t yet — but the pandemic could change that.
The American Council on Education, a national association of colleges and universities, projects that enrollment will drop by 15 percent nationwide next year. Colleges have been refunding room and board charges after sending students home, and canceling commencements and other revenue-generating events.
Those costs are easier to weather for a university like Stanford, with its nearly $28 billion endowment, but could pose an existential crisis for a less-wealthy school, said Douglas Webber, a higher education economist at Temple University.
Think of it as comparing a corporate fast-food chain to a mom-and-pop restaurant, Webber said. “The giant chain is going to be able to find ways to cut back,” he said. “The small family restaurant, with the same percentage hit, it’s going to put them under.”
Nationally, he said, “I would be shocked if there aren’t a lot of closures within the next 12 months.”

Not just bastions of the elite, California’s private, non-profit colleges — which have a median endowment of just over $24 million — award about a fifth of the state’s bachelor’s degrees. About half of their students are the first in their families to attend college, often relying heavily on scholarships and loans to enroll.
When the Association of Independent California Colleges and Universities surveyed its members about the costs of the pandemic, 25 of 85 colleges responded, reporting collective losses of $150 million for the spring semester, Soares said. California’s independent colleges will receive $156 million in total from the federal stimulus bill called the CARES Act, with half the money directed to students as emergency aid and the remainder distributed in various amounts to the colleges. The organization still is tallying losses among independent colleges, Soares said, and has asked state lawmakers to ensure that federal relief money is available to private as well as public schools.
Many colleges have frozen hiring, including Mills College in Oakland, which took “a seven-figure hit” to revenue this year, according to its president, Beth Hillman. The 1,100-student liberal arts college for women and non-binary students has so far managed to avoid layoffs, she said, in part by shifting employees into other roles, like turning athletic coaches into counselors.
(Image: San Francisco Art Institute, founded in 1871, is no longer enrolling new students due to financial pressures in part related to the novel coronavirus pandemic. Photo by Anne Wernikoff for CalMatters)
Mills already had taken steps in recent years to shore up its future. It slashed tuition, worked to attract more transfer students from community colleges, and filled empty dorm spaces with students from nearby, overcrowded UC Berkeley.
While she wasn’t worried about closing, Hillman said she expected the financial pain to worsen in the fall. “There are so many unknowns,” she said. “I don’t know how anybody could be unconcerned at this point.”
Liberal arts colleges often have less experience delivering classes online than large public universities. They are struggling to maintain a sense of community among far-flung students and faculty.
“For our undergraduates, we are a medium-sized liberal arts school focused on transforming students’ lives, so the transition online is challenging to our very purpose,” said Phil Phillips, the chief operating officer at Pepperdine University. “We always say that what goes on outside the classroom is super-important.”
To keep in touch, the Christian university has held Zoom chapel services in which students and faculty share, sometimes tearfully, about challenges like trying to teach online while caring for three small children, Phillips said.
Private colleges could also suffer if economic fallout from the pandemic prompts students to choose schools that are less expensive or closer to home, as some national surveys have found.
Michelle Myers, a college admissions consultant in the Bay Area, said she typically doesn’t hear much from her clients after they receive their admissions offers. But this spring, she has met with almost every high school senior on her list as they reassess their options. Many, she said, are considering taking time off or attending community college in the fall rather than going directly to a four-year school.
“Whether you’re paying for private or in-state public (college), it’s like, ‘Am I really paying this for online classes?’ ” she said. “If it’s a good fit and they really want to go to that school, most of them are thinking, ‘I’m going to try to defer.’ ”
Vince Cuseo, the dean of admission at Occidental College, said he’s also seen an unusually high number of requests to defer admission from students uncertain about the future.
Students are thinking, “’I’ve applied to these institutions and need to plop my money down, (but) I don’t have a sense of what that experience is going to be like in the fall,” Cuseo said.
Adding to the uncertainty is a rule change made last year by the National Association for College Admission Counseling that will allow colleges to continue recruiting students even after they’ve committed to other schools. That means even colleges with May 1 deadlines for students to send in deposits may not know by then what their fall classes will look like. Others are pushing back deadlines in response to the coronavirus.
“It’s one thing to gauge how many students made a commitment to a college in mid-April; it’s another thing to know how many will show up, if they can, in August for orientation,” said Cuseo.
On the plus side, the small size of some private colleges can make it easier for them to react to challenges quickly, Cuseo said. Since prospective students can’t visit campus, Occidental has given them access to videos from online classes being taught this semester and set up virtual panel discussions with current students involved in specific interests like student government and pre-health majors.

The University of the Pacific has made its financial aid packages more attractive with a $1,500-per-year grant for expenses due to the coronavirus, available to new and current students.
And small colleges argue that their low student-to-faculty ratio means more personalized attention, even online.
“When you have a professor with experience in the field who can schedule one-on-one meetings with students regularly, that’s much different than an 1,100-person class where faculty relies on teaching assistants and graduate students to try to have personal connections,” Hillman said.
Colleges that likely have the most to fear from the coronavirus are those that already faced declining enrollment and rising debt before the outbreak — as was the case with San Francisco Art Institute and Notre Dame de Namur.
(Image: The back window of an art studio seen from the street at the San Francisco Art Institute. Photo by Anne Wernikoff for CalMatters)
“COVID accelerated the downward spiral,” San Francisco Art Institute Board Chair Pam Rorke Levy told alumni in a conference call April 20, after the college said it would help students transfer to other schools while it tried to come up with a new business plan.
The college had been discussing possible mergers with three other colleges, including the University of San Francisco, Rorke Levy said. But those negotiations “came to a grinding stop… the minute the shelter-in-place orders happened,” she said.
That left people like Nikolas Schumann, the art student, in a bind. He’s now trying to figure out which schools will accept his credits so he can transfer. The art institute has said it will continue instruction over the summer so students in their final year can graduate — but Schumann worries the plan, like so many others before, will fall through.
“It sucks when you’ve found the school you think is the one for you,” he said, “and it just shuts down.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Radio Update: A California Union Victory, And Increased COVID-19 Testing
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Wednesday, March 6.
 In a victory for unions in California, Gov. Gavin Newsom Wednesday signed an executive order making it easier for essential workers to receive workmen’s compensation during the pandemic. If a worker is exposed to COVID-19 at work, and falls sick, they will be eligible for benefits without having to prove exactly how and when they were exposed.
In a victory for unions in California, Gov. Gavin Newsom Wednesday signed an executive order making it easier for essential workers to receive workmen’s compensation during the pandemic. If a worker is exposed to COVID-19 at work, and falls sick, they will be eligible for benefits without having to prove exactly how and when they were exposed.According the Santa Rosa Press Democrat,“The change shifts the burden of proof that typically falls on workers and instead requires companies to prove employees didn’t get sick at work."
During yesterday’s Coronavirus Town Hall right here on KRCB, Sonoma County Health Officer Dr. Sundari Mase told host Adia White about increased testing. Although the rollout this week has been a little rocky, anyone in the county – symptoms or not – can sign up for a test. But not everyone can get to testing sites. Here's Mase:
Visit LHI.care/covidtesting or call 1-888-634-1123 to schedule an appointment for a coronavirus test.
-
Radio Update: House of Representatives Passes Three-Trillion-Dollar Coronavirus Package

 We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Wednesday, May 20
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Wednesday, May 20 On Friday, Representative Jared Huffman and his Democratic colleagues in the House of Representatives passed a three-trillion-dollar package to ramp up the federal government’s response to the pandemic.
Huffman and the Democrats are also trying to bring the House together, remotely, in order to get back to work. News Director Steve Mencher spoke with Huffman about the details.
(Image: Representative Jared Huffman at a Town Hall in Petaluma in 2017. Credit: Wikimedia Commons.)
To hear more of their conversation, watch our coronavirus Town Hall norcalpublicmedia.org/
coroanvirus. -
Radio Update: Sonoma County Latino Residents 4.5 Times More Likely To Contract COVID-19
 We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, May 18.
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, May 18.Demographic data released last week shows Sonoma County’s Latino residents are 4.5 times more likely to contract the coronavirus than white residents. KRCB’s Adia White spoke with Alegría De La Cruz, chief deputy Sonoma County counsel, about some of the steps the county is taking to address this disparity. Listen here:
To hear more of their conversation, watch our coronavirus Town Hall tomorrow night at 7 p.m. on KRCB TV 22. Submit your questions at norcalpublicmedia.org/
coroanvirus. -
Radio Update: Supervisor Gorin Answers Questions About Fire Season, COVID-19 Testing
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, May 4.
 Sonoma County Supervisor Susan Gorin will join us for Tuesday's virtual town hall at 7 p.m. In our interview, Gorin answers two listener questions — one with concerns about the upcoming fire season, and one with a personal question about whether it's safe to go back to work.
Sonoma County Supervisor Susan Gorin will join us for Tuesday's virtual town hall at 7 p.m. In our interview, Gorin answers two listener questions — one with concerns about the upcoming fire season, and one with a personal question about whether it's safe to go back to work.Listen to her responses here:
Gorin says new COVID testing sites will be available this week in Santa Rosa and Petaluma. You can visit LHI.care/covidtesting to register for a test or call 888-634-1123 to schedule an appointment. Testing is available for everyone, with or without symptoms. Health care workers can still call (707) 565-4667 to schedule a test.
-
Radio Update: Supervisor Gorin Says Some Parks Will Open Wednesday
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, April 27. We hope you join us for our weekly Coronavirus Town Hall Tuesday, April 28 at 7 p.m. We’ll be joined by Ronit Rubinoff, Executive Director, Legal Aid of Sonoma County; Representative Mike Thompson and Assembly Member Jim Wood; a panel of health executives; a report from the South Bay; and our weekly visit from Sonoma County Health Officer Dr. Sundari Mase.
We hope you join us for our weekly Coronavirus Town Hall Tuesday, April 28 at 7 p.m. We’ll be joined by Ronit Rubinoff, Executive Director, Legal Aid of Sonoma County; Representative Mike Thompson and Assembly Member Jim Wood; a panel of health executives; a report from the South Bay; and our weekly visit from Sonoma County Health Officer Dr. Sundari Mase.Chair of the Sonoma County Board of Supervisors, Susan Gorin, will be on the program, announcing some good news about our parks. She talked with news director Steve Mencher Friday evening about how churches are providing connection and when parks will reopen. Listen to the interview to learn more:
-
Reopening in the COVID Era: How to Adapt to a New Normal
By Julie Appleby, Kaiser Health News As many states begin to reopen — most without meeting the thresholds recommended by the White House — a new level of COVID-19 risk analysis begins for Americans.
As many states begin to reopen — most without meeting the thresholds recommended by the White House — a new level of COVID-19 risk analysis begins for Americans.Should I go to the beach? What about the hair salon? A sit-down restaurant meal? Visit Mom on Mother’s Day?
States are responding to the tremendous economic cost of the pandemic and people’s pent-up desire to be “normal” again. But public health experts remain cautious. In many areas, they note, COVID cases — and deaths — are still on the rise, and some fear new surges will follow the easing of restrictions.
“Reopening is not back to normal. It is trying to find ways to allow people to get back out to do things they want to do, and business to do business,” said Dr. Marcus Plescia, chief medical officer at the Association of State and Territorial Health Officials. “We can’t pretend the virus has gone away. The vast majority of the population is still susceptible.”
(Image: Lidvina Mikulic, Army and Air Force Exchange Service concessionaire, helps a customer at the Base Exchange at Ramstein Air Base, Germany, April 21, 2020. U.S. Air Force photo by Senior Airman Elizabeth Baker)
So far, state rules vary. But they involve a basic theme.
“They are making assumptions that people will use common sense and good public health practice when they go out,” said Dr. Georges Benjamin, executive director with the American Public Health Association.
As states start to reopen, people will have to weigh the risk versus benefit of getting out more, along with their own tolerance for uncertainty. The bottom line, health experts say, is people should continue to be vigilant: Maintain distance, wear masks, wash your hands — and take responsibility for your own health and that of those around you.
“It’s clearly too early, in my mind, in many places to pull the stay-at-home rules,” said Benjamin. “But, to the extent that is going to happen, we have to give people advice to do it safely. No one should interpret my comments as being overly supportive of doing it, but if you’re going to do it, you have to be careful.”
An added caveat: All advice applies to people at normal risk of weathering the disease. Those 60 or older and people with underlying health conditions or compromised immune systems should continue staying home.
“Folks who are at higher risk of having a more severe reaction have to continue to be very careful and limit contact with other people,” Plescia said.
So, should I go to the beach?
There’s nothing inherently risky about the beach, said Benjamin. But, again, “if you can, avoid crowds,” he said. “Have as few people around you as possible.”
Maintain that 6-foot distance, even in the water.
“If you are standing close and interacting, there is a chance they could be sick and they may not know it and you could catch it,” Plescia said. “The whole 6-foot distance is a good thing to remember going forward.”
Still, “one thing about the beach or anywhere outside is that there is a lot of good air movement, which is very different than standing in a crowded subway car,” he said.
Even so, recent images of packed beaches and parks raise questions about whether people are able or willing to continue heeding distancing directives.
But if we’re all wearing masks, do we really need to stay 6 feet apart?
Yes, for two reasons. First, while masks can reduce the amount of droplets expelled from the mouth and nose, they aren’t perfect.
Droplets from sneezing, coughing or possibly even talking are considered the main way the coronavirus is transmitted, from landing either on another person or surface. Those who touch that surface may be at risk of infection if they then touch their face, especially the eyes or mouth. “By wearing a mask, I reduce the amount of particles I express out of my mouth,” said Benjamin. “I try to protect you from me, but it also protects me from you.”
And, second, masks don’t protect your eyes. Since the virus can enter the body through the eyes, standing further apart also reduces that risk.
Should I visit Mom on Mother’s Day?
This is a complex choice for many families. Obviously, if Mom is in a nursing home or assisted living, the answer is clearly no, as most care facilities are closed to visitors because the virus has been devastating that population.
There’s still risk beyond such venues. Data from the Centers for Disease Control and Prevention shows 8 out of 10 reported deaths from the coronavirus are among those 65 or older. Underlying conditions, such as heart or lung disease and diabetes, appear to play a role, and older adults are more likely to have such conditions.
So, what if Mom is healthy? There’s no easy answer, public health experts say, because how the virus affects any individual is unpredictable. And visitors may be infected and not know it. An estimated 25% of people show no or few symptoms.
“A virtual gathering is a much safer alternative this year,” said Benjamin.
But if your family insists on an in-person Mother’s Day after weighing Mom’s health (and Dad’s, too, if he’s there), “everyone in the family should do a health check before gathering,” he said. “No one with any COVID symptoms or a fever should participate.”
How prevalent COVID is in your region is also a consideration, experts say, as is how much contact you and your other family members have had with other people.
If you do visit Mom, wear masks and refrain from hugging, kissing or other close contact, Benjamin said.
My hair is a mess. What about going to the salon?
Again, no clear answer. As salons and barbershops reopen in some states, they are taking precautions.
States and professional associations are recommending requiring reservations, limiting the number of customers inside the shop at a given time, installing Plexiglas barriers between stations, cleaning the chairs, sinks and other surfaces often, and having stylists and customers wear masks. Ask what steps your salon is taking.
“Employees should stay home if they are sick or in contact with someone who is sick,” said Dr. Amanda Castel, professor of epidemiology at Milken Institute School of Public Health at the George Washington University. “Also, employers should make sure they don’t have everyone congregating in the kitchen or break room.”
Some salons or barbers are cutting hair outside, she noted, which may reduce the risk because of better ventilation. Salons should also keep track of the customers they see, just in case they need to contact them later, should there be a reason to suspect a client or stylist had become infected, Castel said.
Consider limiting chitchat during the cut, said Plescia, as talking in close proximity may increase your risk, although “it feels a little rude,” he admitted.
What if your stylist is coughing and sneezing?
“I would leave immediately,” he said.
What about dining at a restaurant?
Many states and the CDC have recommendations for restaurants that limit capacity — some states say 25% — in addition to setting tables well apart, using disposable menus and single-serve condiments, and requiring wait staff to wear masks.
“That’s the kind of thing that does help reduce the chance of spread of infection,” Plescia said.
If your favorite eatery is opening, call to ask what precautions are in place. Make a reservation and “be thoughtful about who you are having dinner with,” said Plescia. Household members are one thing, but “getting into closer physical contact with friends is something people should be cautious about.”
Overall, decide how comfortable you are with the concept.
“If you’re going to go to a restaurant just to sit around and worry, then you might as well do takeout,” he said.
And travel?
Consider your options and whether you really need to go, say experts.
Driving and staying in a hotel may be an option for some people.
If hotels are adequately cleaned between guests, “you could make that work,” said Plescia. Bring cleaning wipes and even your own pillows. Again, though, “if you’re going to see an elderly parent, you don’t want to contract something on the way and give it to them.”
Regarding air travel — airlines are taking steps, such as doing deep cleaning between flights. Fresh and recirculated air goes through special HEPA filters. While there is little specific research yet on the coronavirus and air travel, studies on other respiratory and infectious diseases have generally concluded the overall risk is low, except for people within two rows of the infected person. But a case involving an earlier type of coronavirus seemed to indicate wider possible spread across several rows.
Maintaining distance on the plane and in the boarding process is key.
“Wear a mask on the plane,” said Benjamin.
And plan ahead. How prevalent is the coronavirus in the areas you are traveling to and from? Are there any requirements that you self-isolate upon arrival? How will you get to and from the airport while minimizing your proximity to others?
But if it’s not essential, you might want to think twice right now.
“People who absolutely don’t have to travel should avoid doing it,” said Plescia.
Worship services are important to me. What precautions should be considered?
The distance rule applies as houses of worship consider reopening.
“As much as you can within religious rules, try to avoid contact,” said Benjamin.
He is not giving any advice on Holy Communion, saying that is up to religious leaders. But, he noted, “drinking from the same cup raises the risk if a person is sick or items are touched by anyone who is sick.”
Finally, keep in mind that much is being learned about the virus every day, from treatments to side effects to how it spreads.
“My own personal approach is, try to play it on the cautious side a bit longer,” said Plescia.
Castel agreed.
“We need a little more time to fully understand how COVID-19 works and more time to ramp up our testing, find treatments and hopefully a vaccine,” she said. “We all have social distancing fatigue. But we can continue to save lives by doing this.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
-
Santa Clara County Says Shelter-In-Place Appears to Be Working, Provides COVID-19 Updates
 Santa Clara County says sheltering in place appears to be “flattening the curve” — or slowing the rate of coronavirus infection in the county.
Santa Clara County says sheltering in place appears to be “flattening the curve” — or slowing the rate of coronavirus infection in the county. “However, the number of infections is still rising, and we have not yet reached the peak,” says Antoinnae Comeaux, CBO of the county Emergency Operations Center, in a note to community partners. “Our collective efforts are giving health officials more time to plan for a surge in patients and minimize the number of deaths in our County.”
The Public Health Department has expanded its COVID-19 data dashboard to include confirmed cases and deaths by city of residence and deaths by race/ethnicity. Though the county notes that community transmission is believed to be widespread, and case counts represent only a small portion of cases within each city due to limited testing capacity.
Ahead of the Easter holiday, Comeaux asked faith leaders to help keep their communities safe and healthy by reminding congregations about the importance of social distancing.
“In the spirit of the love we have for one another, it is absolutely necessary to keep our distance and stay at home with only the people we live with during this season of religious celebration,” she said.
Comeaux also offered a reminder that disclosures of large inventories of personal protective equipment (PPE) and ventilators by individuals and entities are due to the county, per a public health order, by April 15.
More information can be found on the County Public Health website. Any business, faith, nonprofit, or community leader with questions should contact
This email address is being protected from spambots. You need JavaScript enabled to view it. . -
Santa Rosa CityBus to Further Reduce Service in Response to Pandemic
 The Santa Rosa CityBus will further reduce its service this week to help slow the spread of coronavirus.
The Santa Rosa CityBus will further reduce its service this week to help slow the spread of coronavirus. Starting Monday, April 13, the bus will operate on a Sunday schedule seven days a week for essential travel only. Sunday routes run from about 10 a.m. to 5 p.m.
The only exception will be additional service on Route 1 and Route 2Bto allow for social distancing and reduce overcrowding. Service on Route 10 will be on weekday routing (service to Round Barn) with a weekend timetable.
(Image: Wikipedia Creative Commons)
CityBus will also be providing a special call-ahead service for essential travel Monday through Saturday between 6 a.m. and 10 a.m., and 5 p.m. and 8 p.m. This service will be provided by the City’s paratransit contractor, MV Transportation, but is open to the general public with the following guidelines:
- This service is for riders who MUST travel to either a job at an essential service provider or to an essential destination within the city of Santa Rosa.
- Riders must call ahead to 707-546-1999 to register for this service and schedule this trip.
- Riders registering for this service will need to provide their name, home address, contact information and destination address trip. Once registered for the service, riders can schedule a trip up to seven days in advance of the trip but at a minimum must schedule their trip the day before between the hours of 8 a.m. and 5 p.m., Monday-Saturday, or between the hours of 9 a.m. and 3 p.m. on Sundays.
- Riders must call to cancel trips at least two hours in advance in order to continue receiving this service.
- Language assistance is available to any non-English speakers who wish to schedule trips.
- Due to limited capacity, trips may be prioritized or further limited in the future.
Santa Rosa Paratransit will continue to operate regular weekday, Saturday and Sunday service hours for essential travel. And Route 16 (Oakmont) will continue to operate for essential travel.
Find more details here. -
Santa Rosa Fire Department Creates Pandemic Response Unit

The Santa Rosa Fire Department has created a new Pandemic Response Unit to respond to patients suspected of having COVID-19 or that are experiencing flu-like symptoms within the city.
The department says the new squad, which had its first shift Tuesday, was established in an effort to minimize department and community exposure to the virus.
The Pandemic Response Unit vehicle, “SQUAD 1,” is equipped with specialized personal protective equipment and advanced life support gear and is staffed by one paramedic and one emergency medical technician (EMT) from the fire department. The department says this unit is one of the first of its kind in California.
(Image: Santa Rosa firefighters wear blue in honor of Detective Marylou Armer who died from COVID-19 / Credit Santa Rosa Fire Department Twitter).
“This is a proactive and innovative method to reduce exposure to the coronavirus and limit the possibility of a widespread infection within our community, our Department, and the families of our staff," Santa Rosa Fire Chief Tony Gossner said.
Fire personnel that are a part of the response unit will wear additional personal protective equipment, minimize contact with potentially infected patients and will decontaminate before leaving the location of any emergency call, the department says.
The unit is available 24/7 and will operate indefinitely.
To learn more, watch a community update video from Chief Gossner in English or Spanish, or listen to KRCB’s Adia White speaking with Deputy Fire Chief Scott Westrope about how many calls the team has responded to so far.
-
Santa Rosa To Use City Parking Lot To House Homeless In Tents During Pandemic
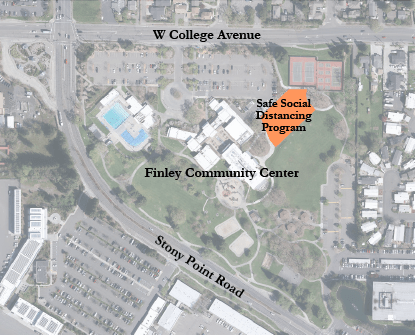 Santa Rosa will soon be making use of a city-owned parking lot to house people experiencing homelessness in tents.
Santa Rosa will soon be making use of a city-owned parking lot to house people experiencing homelessness in tents.The goal is to provide a space where people living without shelter can maintain safe social distance amid the coronavirus pandemic.
The parking lot at Finley Community Center will include up to 70 tents, spaced 12 feet apart, with each tent accommodating an individual or couple.
The tents will be provided by the city, and portable toilets, hand-washing stations, meal delivery, on-site management and services will be coordinated by Catholic Charities staff. Overnight on-site security will also be provided.
“We are moving forward with this emergency temporary measure given the urgent need to protect the City’s unsheltered homeless community as they are some of the most vulnerable to the spread of the coronavirus,” Mayor Tom Schwedhelm said in a press release. “This new, managed site offers a safer, temporary option for those who have been living outdoors in situations where social distancing is challenging if not impossible.”
Setup of the site is anticipated to begin the week of May 11, with occupancy likely beginning the week of May 18 and lasting through the duration of the county’s shelter-in-place order.
The 24,600-square-foot parking lot is located between the Person Senior Wing building and the Finley tennis courts.
More information about homeless support during the COVID-19 pandemic can be found at https://srcity.org/3284/Homelessness-Services.
Page 1 of 2
Northern California
Public Media
Newsletter
Get the latest updates on programs and events.

 Live Radio
Live Radio
