Hearken1 English
-
Predicting a Pandemic’s Path: What Models Can and Can’t Do
ByBarbara Feder Ostrov, CalMatters
 Every day, while we’re all stuck at home, politicians and health officials and news anchors point to graphics showing the latest statistics on the coronavirus pandemic to indicate what might happen next, in your region and around the world.
Every day, while we’re all stuck at home, politicians and health officials and news anchors point to graphics showing the latest statistics on the coronavirus pandemic to indicate what might happen next, in your region and around the world. Underlying those visuals are disease forecasting models — complex mathematical algorithms that predict disease spread and severity based on different scenarios. Because they can help predict the effects of different interventions, including our social distancing, coronavirus pandemic models significantly influence how governments are responding.
It’s tempting to regard these models as oracles that can tell us precisely what to do and when to do it. Can they tell us when we should return to work, or when our kids can go back to school? Is Grandma safe in her nursing home or should she come home? When can businesses safely reopen?
As California’s COVID-19 caseload tops 30,000, state officials are using a model developed at Johns Hopkins University to aid in their planning. If you’ve watched Gov. Gavin Newsom’s daily briefings online, some of the charts shown are based on the model’s predictions.
But the models need to be fed reliable data, and some data is in short supply, especially without widespread U.S. testing for the novel coronavirus that causes COVID-19. We still don’t know how many people have been infected without symptoms, for example. Other inputs, such as incubation periods and death rates, change by the day as we learn more about this virus.
“What makes modeling especially challenging are the human factors. Individual behaviors, health care infrastructure and political response each can affect the outcome of an epidemic,” said Shweta Bansal, an associate professor of biology at Georgetown University who specializes in disease modeling. “I think of models as a call to action. They can tell us what happens if we don’t act and how we can prevent the most dire consequences.”
Here are five things you should know to make sense of infectious disease models:
Why are there so many COVID pandemic models — and why are they all so different?
There are different types of infectious disease models for different purposes. Each has limitations and each can be useful in its own way.
“SEIR” models, for example, involve equations based on the number of susceptible people (S) who can be infected, the number of people exposed (E), the number of people infected (I) and the number of people recovered(R). Agent-based models use massive computer power to simulate the actions of millions of hypothetical people to predict the spread of disease. Still other models examine a disease outbreak in one country and try to predict outcomes elsewhere in the world based on that data. Some models look at travel patterns in spreading disease, and still others assess how age, ethnicity and contributing illnesses may affect survival rates.
Epidemiologists say it helps to have more than one model in responding to disease outbreaks because they use different inputs. Combining results from multiple models can give a more nuanced picture of an outbreak’s trajectory.
“The fact that there are so many models is a healthy sign,” said Bansal. “It’s the same with weather forecasts that rely on multiple mathematical models. But unlike a weather forecast, with a disease forecast we have the ability to change the outcome.”
The White House has controversially used a model developed by the University of Washington’s Institute for Health Metrics and Evaluation, which some disease experts have criticized as being based on overly optimistic assumptions about the benefits of social distancing, among other statistical issues. The Imperial College London model, which predicted as many as 22 million U.S. deaths if no action was taken, also apparently prompted the Trump administration to issue tougher new social distancing guidelines.
What goes into making an epidemiological model for an infectious respiratory disease?California and some other states use an SEIR model developed by Johns Hopkins University epidemiologist Dr. Justin Lessler. This coronavirus pandemic model, according to the California Department of Public Health, takes into account assumptions about how long the disease takes to incubate, how long people are infectious, how many people each patient can infect, the fatality rate, how many people need hospitalization or intensive care, and importantly for hospital planning, how many people need ventilators because they can’t breathe on their own.
The model assumes that NPIs – “non-pharmaceutical interventions” such as social distancing – started in the state March 20. In fact, some counties ordered residents to shelter in place earlier, some later.
California also has been faring better on a daily basis than this model’s predictions had forecasted — only 4,892 cases were reported on April 16, compared to 12,119 cases projected for that date. Assembly members set aside time at a budget hearing Monday to question the Newsom administration about the model and seek more details about its assumptions.
Rodger Butler, a spokesman for the California Health and Human Services Agency, cautioned that “there is considerable uncertainty” in the model’s predictions because we still don’t know enough about how the virus behaves and, without widespread testing, how many people are infected. “We are continuously refining our model with researchers and local public health offices,” Butler said.
Which raises the next question:
What happens if you don’t have enough data, or the right data?
This is what keeps public health experts up at night.
Because testing has lagged so badly in the United States, “right now we don’t know how many people are infected,” said Karin Michels, professor and chair of the epidemiology department at UCLA’s School of Public Health. “The biggest unknown (for disease models) is the denominator. How many people out of the infected are actually dying or wind up in the ICU? We have no idea at this point.”
Epidemiologists want to know more about when people are no longer infectious. They hope to learn more about who, once infected, is most likely to need hospitalization or a ventilator, to prevent overwhelming hospitals. True fatality rates aren’t one-size-fits-all; they will differ by age, gender, underlying illness and access to health care, among other factors.
Epidemiologists also need to better understand how many people might have been infected but not show symptoms. New antibody tests now being rolled out can help answer that question, but not quickly, and some of these tests are proving inaccurate. Some public health experts say that preventable delays in widespread testing and a perceived chaotic federal response have prevented the kind of critical data gathering needed to get a handle on outbreaks in various regions of the country — and to provide the kind of intelligence needed before reopening the country.
What makes a model succeed in its predictions?
Disease modelers and mathematicians argue about this a lot. The quality of the data that goes into a disease model is important. The range of error in the model’s predictions are important, too. If early predictions of a model don’t measure up to reality, its later predictions may not as well.
The University of Washington’s coronavirus pandemic model, for example, which aimed to predict outbreaks based primarily on early data from China and later Europe, has had such a wide range of error in its predicted death rates that some epidemiologists have recommended that governments do not use it for planning. The model’s predictions of when cases will peak in various regions also have swung dramatically in different weeks — and rarely coincided with other models’ forecasts, prompting some experts’ concern about the model’s validity going forward. Some politicians are citing the model’s relatively optimistic forecasts as justification to open the country earlier than public health officials recommend.
The model’s developers say they are continually updating their model and have adjusted it to reflect regional differences in how daily death rates peak over time, and how social distancing policies vary by region.
Still, disease models are supposed to serve as a wake-up call prompting us to act. If our actions succeed in slowing infections and deaths, making the predictions inaccurate — that’s a good thing.
What do public health experts wish people understood about coronavirus pandemic models?
Disease models are not perfect, and they can adapt as new data becomes available. Models “can help us think through different scenarios, but they shouldn’t be used as crystal balls,” Bansal said. “If we believe that a model’s prediction of 100,000 deaths is what will happen if we don’t act, then we do everything we can to prevent those 100,000 deaths.”
Also: they’re better for predicting short-term needs and outcomes, Michels said, such as how many ventilators a hospital might need next month, rather than next year:
“I don’t think we can predict the fall yet. We only know the virus will still be around, so life will be complicated.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Private Colleges Brace for Downturn Amid Pandemic Fallout
ByFelicia Mello, CalMatters
 Nikolas Schumann was a community college student and budding painter when he first learned about the San Francisco Art Institute from a mentor. He visited the school, “absolutely loved” it, and decided to transfer there in 2018 after a large scholarship knocked his tuition from $46,000 per year down to $15,000.
Nikolas Schumann was a community college student and budding painter when he first learned about the San Francisco Art Institute from a mentor. He visited the school, “absolutely loved” it, and decided to transfer there in 2018 after a large scholarship knocked his tuition from $46,000 per year down to $15,000. “It just had so much history and was so diverse,” Schumann said. “They birth interesting and wild artists.”
But just a few months from graduation, Schumann’s plans are in limbo after the art institute, along with another Bay Area college, Notre Dame de Namur University, said last month they would not be enrolling any new students in the fall. Art institute officials cited the coronavirus outbreak as a factor in their decision.
The news from the two schools — one a Catholic university that was the first in California to admit women in 1868, the other a fine arts academy that counts photographer Annie Leibovitz among its alumni — highlights the financial challenges facing the state’s small private colleges as the pandemic imposes new costs and throws the admissions cycle into turmoil.
(Image: Painting major Nikolas Schumann picks up a canvas from the closed Chestnut Street campus of San Francisco Art Institute. Schumann says he will likely transfer to California College of the Arts next year to finish his degree. Photo by Anne Wernikoff for CalMatters)
Unlike public universities like the University of California system, private colleges cannot count on state tax dollars to keep them afloat. Many of their most attractive selling points, from charming campuses to face time with professors, no longer apply in a world where instruction has moved online. With families less willing and able to pay tuition that can reach $50,000 per year for what some have dubbed ‘Zoom University,’ the pandemic has raised fears that a growing number of independent colleges could scale back, merge or even shut down.
“Most schools do not have large endowments that could provide the rainy day fund that we need right now,” said Kristen Soares, executive director of the Association of Independent California Colleges and Universities, which represents private, non-profit colleges. “If this goes into the fall, it could be very devastating.”
Most at risk, experts say: less-selective residential colleges that are not well-known outside their local area. The Midwest and Northeast have seen a wave of closures among such schools. California, with its larger population of college-ready high school graduates, hasn’t yet — but the pandemic could change that.
The American Council on Education, a national association of colleges and universities, projects that enrollment will drop by 15 percent nationwide next year. Colleges have been refunding room and board charges after sending students home, and canceling commencements and other revenue-generating events.
Those costs are easier to weather for a university like Stanford, with its nearly $28 billion endowment, but could pose an existential crisis for a less-wealthy school, said Douglas Webber, a higher education economist at Temple University.
Think of it as comparing a corporate fast-food chain to a mom-and-pop restaurant, Webber said. “The giant chain is going to be able to find ways to cut back,” he said. “The small family restaurant, with the same percentage hit, it’s going to put them under.”
Nationally, he said, “I would be shocked if there aren’t a lot of closures within the next 12 months.”

Not just bastions of the elite, California’s private, non-profit colleges — which have a median endowment of just over $24 million — award about a fifth of the state’s bachelor’s degrees. About half of their students are the first in their families to attend college, often relying heavily on scholarships and loans to enroll.
When the Association of Independent California Colleges and Universities surveyed its members about the costs of the pandemic, 25 of 85 colleges responded, reporting collective losses of $150 million for the spring semester, Soares said. California’s independent colleges will receive $156 million in total from the federal stimulus bill called the CARES Act, with half the money directed to students as emergency aid and the remainder distributed in various amounts to the colleges. The organization still is tallying losses among independent colleges, Soares said, and has asked state lawmakers to ensure that federal relief money is available to private as well as public schools.
Many colleges have frozen hiring, including Mills College in Oakland, which took “a seven-figure hit” to revenue this year, according to its president, Beth Hillman. The 1,100-student liberal arts college for women and non-binary students has so far managed to avoid layoffs, she said, in part by shifting employees into other roles, like turning athletic coaches into counselors.
(Image: San Francisco Art Institute, founded in 1871, is no longer enrolling new students due to financial pressures in part related to the novel coronavirus pandemic. Photo by Anne Wernikoff for CalMatters)
Mills already had taken steps in recent years to shore up its future. It slashed tuition, worked to attract more transfer students from community colleges, and filled empty dorm spaces with students from nearby, overcrowded UC Berkeley.
While she wasn’t worried about closing, Hillman said she expected the financial pain to worsen in the fall. “There are so many unknowns,” she said. “I don’t know how anybody could be unconcerned at this point.”
Liberal arts colleges often have less experience delivering classes online than large public universities. They are struggling to maintain a sense of community among far-flung students and faculty.
“For our undergraduates, we are a medium-sized liberal arts school focused on transforming students’ lives, so the transition online is challenging to our very purpose,” said Phil Phillips, the chief operating officer at Pepperdine University. “We always say that what goes on outside the classroom is super-important.”
To keep in touch, the Christian university has held Zoom chapel services in which students and faculty share, sometimes tearfully, about challenges like trying to teach online while caring for three small children, Phillips said.
Private colleges could also suffer if economic fallout from the pandemic prompts students to choose schools that are less expensive or closer to home, as some national surveys have found.
Michelle Myers, a college admissions consultant in the Bay Area, said she typically doesn’t hear much from her clients after they receive their admissions offers. But this spring, she has met with almost every high school senior on her list as they reassess their options. Many, she said, are considering taking time off or attending community college in the fall rather than going directly to a four-year school.
“Whether you’re paying for private or in-state public (college), it’s like, ‘Am I really paying this for online classes?’ ” she said. “If it’s a good fit and they really want to go to that school, most of them are thinking, ‘I’m going to try to defer.’ ”
Vince Cuseo, the dean of admission at Occidental College, said he’s also seen an unusually high number of requests to defer admission from students uncertain about the future.
Students are thinking, “’I’ve applied to these institutions and need to plop my money down, (but) I don’t have a sense of what that experience is going to be like in the fall,” Cuseo said.
Adding to the uncertainty is a rule change made last year by the National Association for College Admission Counseling that will allow colleges to continue recruiting students even after they’ve committed to other schools. That means even colleges with May 1 deadlines for students to send in deposits may not know by then what their fall classes will look like. Others are pushing back deadlines in response to the coronavirus.
“It’s one thing to gauge how many students made a commitment to a college in mid-April; it’s another thing to know how many will show up, if they can, in August for orientation,” said Cuseo.
On the plus side, the small size of some private colleges can make it easier for them to react to challenges quickly, Cuseo said. Since prospective students can’t visit campus, Occidental has given them access to videos from online classes being taught this semester and set up virtual panel discussions with current students involved in specific interests like student government and pre-health majors.

The University of the Pacific has made its financial aid packages more attractive with a $1,500-per-year grant for expenses due to the coronavirus, available to new and current students.
And small colleges argue that their low student-to-faculty ratio means more personalized attention, even online.
“When you have a professor with experience in the field who can schedule one-on-one meetings with students regularly, that’s much different than an 1,100-person class where faculty relies on teaching assistants and graduate students to try to have personal connections,” Hillman said.
Colleges that likely have the most to fear from the coronavirus are those that already faced declining enrollment and rising debt before the outbreak — as was the case with San Francisco Art Institute and Notre Dame de Namur.
(Image: The back window of an art studio seen from the street at the San Francisco Art Institute. Photo by Anne Wernikoff for CalMatters)
“COVID accelerated the downward spiral,” San Francisco Art Institute Board Chair Pam Rorke Levy told alumni in a conference call April 20, after the college said it would help students transfer to other schools while it tried to come up with a new business plan.
The college had been discussing possible mergers with three other colleges, including the University of San Francisco, Rorke Levy said. But those negotiations “came to a grinding stop… the minute the shelter-in-place orders happened,” she said.
That left people like Nikolas Schumann, the art student, in a bind. He’s now trying to figure out which schools will accept his credits so he can transfer. The art institute has said it will continue instruction over the summer so students in their final year can graduate — but Schumann worries the plan, like so many others before, will fall through.
“It sucks when you’ve found the school you think is the one for you,” he said, “and it just shuts down.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Radio Update: A California Union Victory, And Increased COVID-19 Testing
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Wednesday, March 6.
 In a victory for unions in California, Gov. Gavin Newsom Wednesday signed an executive order making it easier for essential workers to receive workmen’s compensation during the pandemic. If a worker is exposed to COVID-19 at work, and falls sick, they will be eligible for benefits without having to prove exactly how and when they were exposed.
In a victory for unions in California, Gov. Gavin Newsom Wednesday signed an executive order making it easier for essential workers to receive workmen’s compensation during the pandemic. If a worker is exposed to COVID-19 at work, and falls sick, they will be eligible for benefits without having to prove exactly how and when they were exposed.According the Santa Rosa Press Democrat,“The change shifts the burden of proof that typically falls on workers and instead requires companies to prove employees didn’t get sick at work."
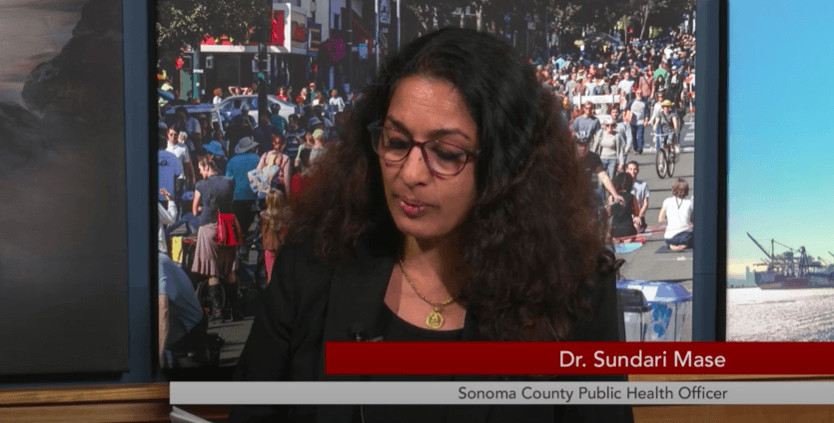
During yesterday’s Coronavirus Town Hall right here on KRCB, Sonoma County Health Officer Dr. Sundari Mase told host Adia White about increased testing. Although the rollout this week has been a little rocky, anyone in the county – symptoms or not – can sign up for a test. But not everyone can get to testing sites. Here's Mase:
Visit LHI.care/covidtesting or call 1-888-634-1123 to schedule an appointment for a coronavirus test.
-
Radio Update: House of Representatives Passes Three-Trillion-Dollar Coronavirus Package

 We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Wednesday, May 20
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Wednesday, May 20 On Friday, Representative Jared Huffman and his Democratic colleagues in the House of Representatives passed a three-trillion-dollar package to ramp up the federal government’s response to the pandemic.
Huffman and the Democrats are also trying to bring the House together, remotely, in order to get back to work. News Director Steve Mencher spoke with Huffman about the details.
(Image: Representative Jared Huffman at a Town Hall in Petaluma in 2017. Credit: Wikimedia Commons.)
To hear more of their conversation, watch our coronavirus Town Hall norcalpublicmedia.org/
coroanvirus. -
Radio Update: Sonoma County Latino Residents 4.5 Times More Likely To Contract COVID-19
 We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, May 18.
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, May 18.Demographic data released last week shows Sonoma County’s Latino residents are 4.5 times more likely to contract the coronavirus than white residents. KRCB’s Adia White spoke with Alegría De La Cruz, chief deputy Sonoma County counsel, about some of the steps the county is taking to address this disparity. Listen here:
To hear more of their conversation, watch our coronavirus Town Hall tomorrow night at 7 p.m. on KRCB TV 22. Submit your questions at norcalpublicmedia.org/
coroanvirus. -
Radio Update: Supervisor Gorin Answers Questions About Fire Season, COVID-19 Testing
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, May 4.
 Sonoma County Supervisor Susan Gorin will join us for Tuesday's virtual town hall at 7 p.m. In our interview, Gorin answers two listener questions — one with concerns about the upcoming fire season, and one with a personal question about whether it's safe to go back to work.
Sonoma County Supervisor Susan Gorin will join us for Tuesday's virtual town hall at 7 p.m. In our interview, Gorin answers two listener questions — one with concerns about the upcoming fire season, and one with a personal question about whether it's safe to go back to work.Listen to her responses here:
Gorin says new COVID testing sites will be available this week in Santa Rosa and Petaluma. You can visit LHI.care/covidtesting to register for a test or call 888-634-1123 to schedule an appointment. Testing is available for everyone, with or without symptoms. Health care workers can still call (707) 565-4667 to schedule a test.
-
Radio Update: Supervisor Gorin Says Some Parks Will Open Wednesday
We provide daily coronavirus updates on KRCB radio 91. Tune in at 9 a.m. and 6:44 p.m. for the latest local news. Here's our update for Monday, April 27. We hope you join us for our weekly Coronavirus Town Hall Tuesday, April 28 at 7 p.m. We’ll be joined by Ronit Rubinoff, Executive Director, Legal Aid of Sonoma County; Representative Mike Thompson and Assembly Member Jim Wood; a panel of health executives; a report from the South Bay; and our weekly visit from Sonoma County Health Officer Dr. Sundari Mase.
We hope you join us for our weekly Coronavirus Town Hall Tuesday, April 28 at 7 p.m. We’ll be joined by Ronit Rubinoff, Executive Director, Legal Aid of Sonoma County; Representative Mike Thompson and Assembly Member Jim Wood; a panel of health executives; a report from the South Bay; and our weekly visit from Sonoma County Health Officer Dr. Sundari Mase.Chair of the Sonoma County Board of Supervisors, Susan Gorin, will be on the program, announcing some good news about our parks. She talked with news director Steve Mencher Friday evening about how churches are providing connection and when parks will reopen. Listen to the interview to learn more:
-
Reopening in the COVID Era: How to Adapt to a New Normal
By Julie Appleby, Kaiser Health News As many states begin to reopen — most without meeting the thresholds recommended by the White House — a new level of COVID-19 risk analysis begins for Americans.
As many states begin to reopen — most without meeting the thresholds recommended by the White House — a new level of COVID-19 risk analysis begins for Americans.Should I go to the beach? What about the hair salon? A sit-down restaurant meal? Visit Mom on Mother’s Day?
States are responding to the tremendous economic cost of the pandemic and people’s pent-up desire to be “normal” again. But public health experts remain cautious. In many areas, they note, COVID cases — and deaths — are still on the rise, and some fear new surges will follow the easing of restrictions.
“Reopening is not back to normal. It is trying to find ways to allow people to get back out to do things they want to do, and business to do business,” said Dr. Marcus Plescia, chief medical officer at the Association of State and Territorial Health Officials. “We can’t pretend the virus has gone away. The vast majority of the population is still susceptible.”
(Image: Lidvina Mikulic, Army and Air Force Exchange Service concessionaire, helps a customer at the Base Exchange at Ramstein Air Base, Germany, April 21, 2020. U.S. Air Force photo by Senior Airman Elizabeth Baker)
So far, state rules vary. But they involve a basic theme.
“They are making assumptions that people will use common sense and good public health practice when they go out,” said Dr. Georges Benjamin, executive director with the American Public Health Association.
As states start to reopen, people will have to weigh the risk versus benefit of getting out more, along with their own tolerance for uncertainty. The bottom line, health experts say, is people should continue to be vigilant: Maintain distance, wear masks, wash your hands — and take responsibility for your own health and that of those around you.
“It’s clearly too early, in my mind, in many places to pull the stay-at-home rules,” said Benjamin. “But, to the extent that is going to happen, we have to give people advice to do it safely. No one should interpret my comments as being overly supportive of doing it, but if you’re going to do it, you have to be careful.”
An added caveat: All advice applies to people at normal risk of weathering the disease. Those 60 or older and people with underlying health conditions or compromised immune systems should continue staying home.
“Folks who are at higher risk of having a more severe reaction have to continue to be very careful and limit contact with other people,” Plescia said.
So, should I go to the beach?
There’s nothing inherently risky about the beach, said Benjamin. But, again, “if you can, avoid crowds,” he said. “Have as few people around you as possible.”
Maintain that 6-foot distance, even in the water.
“If you are standing close and interacting, there is a chance they could be sick and they may not know it and you could catch it,” Plescia said. “The whole 6-foot distance is a good thing to remember going forward.”
Still, “one thing about the beach or anywhere outside is that there is a lot of good air movement, which is very different than standing in a crowded subway car,” he said.
Even so, recent images of packed beaches and parks raise questions about whether people are able or willing to continue heeding distancing directives.
But if we’re all wearing masks, do we really need to stay 6 feet apart?
Yes, for two reasons. First, while masks can reduce the amount of droplets expelled from the mouth and nose, they aren’t perfect.
Droplets from sneezing, coughing or possibly even talking are considered the main way the coronavirus is transmitted, from landing either on another person or surface. Those who touch that surface may be at risk of infection if they then touch their face, especially the eyes or mouth. “By wearing a mask, I reduce the amount of particles I express out of my mouth,” said Benjamin. “I try to protect you from me, but it also protects me from you.”
And, second, masks don’t protect your eyes. Since the virus can enter the body through the eyes, standing further apart also reduces that risk.
Should I visit Mom on Mother’s Day?
This is a complex choice for many families. Obviously, if Mom is in a nursing home or assisted living, the answer is clearly no, as most care facilities are closed to visitors because the virus has been devastating that population.
There’s still risk beyond such venues. Data from the Centers for Disease Control and Prevention shows 8 out of 10 reported deaths from the coronavirus are among those 65 or older. Underlying conditions, such as heart or lung disease and diabetes, appear to play a role, and older adults are more likely to have such conditions.
So, what if Mom is healthy? There’s no easy answer, public health experts say, because how the virus affects any individual is unpredictable. And visitors may be infected and not know it. An estimated 25% of people show no or few symptoms.
“A virtual gathering is a much safer alternative this year,” said Benjamin.
But if your family insists on an in-person Mother’s Day after weighing Mom’s health (and Dad’s, too, if he’s there), “everyone in the family should do a health check before gathering,” he said. “No one with any COVID symptoms or a fever should participate.”
How prevalent COVID is in your region is also a consideration, experts say, as is how much contact you and your other family members have had with other people.
If you do visit Mom, wear masks and refrain from hugging, kissing or other close contact, Benjamin said.
My hair is a mess. What about going to the salon?
Again, no clear answer. As salons and barbershops reopen in some states, they are taking precautions.
States and professional associations are recommending requiring reservations, limiting the number of customers inside the shop at a given time, installing Plexiglas barriers between stations, cleaning the chairs, sinks and other surfaces often, and having stylists and customers wear masks. Ask what steps your salon is taking.
“Employees should stay home if they are sick or in contact with someone who is sick,” said Dr. Amanda Castel, professor of epidemiology at Milken Institute School of Public Health at the George Washington University. “Also, employers should make sure they don’t have everyone congregating in the kitchen or break room.”
Some salons or barbers are cutting hair outside, she noted, which may reduce the risk because of better ventilation. Salons should also keep track of the customers they see, just in case they need to contact them later, should there be a reason to suspect a client or stylist had become infected, Castel said.
Consider limiting chitchat during the cut, said Plescia, as talking in close proximity may increase your risk, although “it feels a little rude,” he admitted.
What if your stylist is coughing and sneezing?
“I would leave immediately,” he said.
What about dining at a restaurant?
Many states and the CDC have recommendations for restaurants that limit capacity — some states say 25% — in addition to setting tables well apart, using disposable menus and single-serve condiments, and requiring wait staff to wear masks.
“That’s the kind of thing that does help reduce the chance of spread of infection,” Plescia said.
If your favorite eatery is opening, call to ask what precautions are in place. Make a reservation and “be thoughtful about who you are having dinner with,” said Plescia. Household members are one thing, but “getting into closer physical contact with friends is something people should be cautious about.”
Overall, decide how comfortable you are with the concept.
“If you’re going to go to a restaurant just to sit around and worry, then you might as well do takeout,” he said.
And travel?
Consider your options and whether you really need to go, say experts.
Driving and staying in a hotel may be an option for some people.
If hotels are adequately cleaned between guests, “you could make that work,” said Plescia. Bring cleaning wipes and even your own pillows. Again, though, “if you’re going to see an elderly parent, you don’t want to contract something on the way and give it to them.”
Regarding air travel — airlines are taking steps, such as doing deep cleaning between flights. Fresh and recirculated air goes through special HEPA filters. While there is little specific research yet on the coronavirus and air travel, studies on other respiratory and infectious diseases have generally concluded the overall risk is low, except for people within two rows of the infected person. But a case involving an earlier type of coronavirus seemed to indicate wider possible spread across several rows.
Maintaining distance on the plane and in the boarding process is key.
“Wear a mask on the plane,” said Benjamin.
And plan ahead. How prevalent is the coronavirus in the areas you are traveling to and from? Are there any requirements that you self-isolate upon arrival? How will you get to and from the airport while minimizing your proximity to others?
But if it’s not essential, you might want to think twice right now.
“People who absolutely don’t have to travel should avoid doing it,” said Plescia.
Worship services are important to me. What precautions should be considered?
The distance rule applies as houses of worship consider reopening.
“As much as you can within religious rules, try to avoid contact,” said Benjamin.
He is not giving any advice on Holy Communion, saying that is up to religious leaders. But, he noted, “drinking from the same cup raises the risk if a person is sick or items are touched by anyone who is sick.”
Finally, keep in mind that much is being learned about the virus every day, from treatments to side effects to how it spreads.
“My own personal approach is, try to play it on the cautious side a bit longer,” said Plescia.
Castel agreed.
“We need a little more time to fully understand how COVID-19 works and more time to ramp up our testing, find treatments and hopefully a vaccine,” she said. “We all have social distancing fatigue. But we can continue to save lives by doing this.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
-
Santa Clara County Says Shelter-In-Place Appears to Be Working, Provides COVID-19 Updates
 Santa Clara County says sheltering in place appears to be “flattening the curve” — or slowing the rate of coronavirus infection in the county.
Santa Clara County says sheltering in place appears to be “flattening the curve” — or slowing the rate of coronavirus infection in the county. “However, the number of infections is still rising, and we have not yet reached the peak,” says Antoinnae Comeaux, CBO of the county Emergency Operations Center, in a note to community partners. “Our collective efforts are giving health officials more time to plan for a surge in patients and minimize the number of deaths in our County.”
The Public Health Department has expanded its COVID-19 data dashboard to include confirmed cases and deaths by city of residence and deaths by race/ethnicity. Though the county notes that community transmission is believed to be widespread, and case counts represent only a small portion of cases within each city due to limited testing capacity.
Ahead of the Easter holiday, Comeaux asked faith leaders to help keep their communities safe and healthy by reminding congregations about the importance of social distancing.
“In the spirit of the love we have for one another, it is absolutely necessary to keep our distance and stay at home with only the people we live with during this season of religious celebration,” she said.
Comeaux also offered a reminder that disclosures of large inventories of personal protective equipment (PPE) and ventilators by individuals and entities are due to the county, per a public health order, by April 15.
More information can be found on the County Public Health website. Any business, faith, nonprofit, or community leader with questions should contact
This email address is being protected from spambots. You need JavaScript enabled to view it. . -
Santa Rosa CityBus to Further Reduce Service in Response to Pandemic
 The Santa Rosa CityBus will further reduce its service this week to help slow the spread of coronavirus.
The Santa Rosa CityBus will further reduce its service this week to help slow the spread of coronavirus. Starting Monday, April 13, the bus will operate on a Sunday schedule seven days a week for essential travel only. Sunday routes run from about 10 a.m. to 5 p.m.
The only exception will be additional service on Route 1 and Route 2Bto allow for social distancing and reduce overcrowding. Service on Route 10 will be on weekday routing (service to Round Barn) with a weekend timetable.
(Image: Wikipedia Creative Commons)
CityBus will also be providing a special call-ahead service for essential travel Monday through Saturday between 6 a.m. and 10 a.m., and 5 p.m. and 8 p.m. This service will be provided by the City’s paratransit contractor, MV Transportation, but is open to the general public with the following guidelines:
- This service is for riders who MUST travel to either a job at an essential service provider or to an essential destination within the city of Santa Rosa.
- Riders must call ahead to 707-546-1999 to register for this service and schedule this trip.
- Riders registering for this service will need to provide their name, home address, contact information and destination address trip. Once registered for the service, riders can schedule a trip up to seven days in advance of the trip but at a minimum must schedule their trip the day before between the hours of 8 a.m. and 5 p.m., Monday-Saturday, or between the hours of 9 a.m. and 3 p.m. on Sundays.
- Riders must call to cancel trips at least two hours in advance in order to continue receiving this service.
- Language assistance is available to any non-English speakers who wish to schedule trips.
- Due to limited capacity, trips may be prioritized or further limited in the future.
Santa Rosa Paratransit will continue to operate regular weekday, Saturday and Sunday service hours for essential travel. And Route 16 (Oakmont) will continue to operate for essential travel.
Find more details here. -
Santa Rosa Fire Department Creates Pandemic Response Unit

The Santa Rosa Fire Department has created a new Pandemic Response Unit to respond to patients suspected of having COVID-19 or that are experiencing flu-like symptoms within the city.
The department says the new squad, which had its first shift Tuesday, was established in an effort to minimize department and community exposure to the virus.
The Pandemic Response Unit vehicle, “SQUAD 1,” is equipped with specialized personal protective equipment and advanced life support gear and is staffed by one paramedic and one emergency medical technician (EMT) from the fire department. The department says this unit is one of the first of its kind in California.
(Image: Santa Rosa firefighters wear blue in honor of Detective Marylou Armer who died from COVID-19 / Credit Santa Rosa Fire Department Twitter).
“This is a proactive and innovative method to reduce exposure to the coronavirus and limit the possibility of a widespread infection within our community, our Department, and the families of our staff," Santa Rosa Fire Chief Tony Gossner said.
Fire personnel that are a part of the response unit will wear additional personal protective equipment, minimize contact with potentially infected patients and will decontaminate before leaving the location of any emergency call, the department says.
The unit is available 24/7 and will operate indefinitely.
To learn more, watch a community update video from Chief Gossner in English or Spanish, or listen to KRCB’s Adia White speaking with Deputy Fire Chief Scott Westrope about how many calls the team has responded to so far.
-
Santa Rosa To Use City Parking Lot To House Homeless In Tents During Pandemic
 Santa Rosa will soon be making use of a city-owned parking lot to house people experiencing homelessness in tents.
Santa Rosa will soon be making use of a city-owned parking lot to house people experiencing homelessness in tents.The goal is to provide a space where people living without shelter can maintain safe social distance amid the coronavirus pandemic.
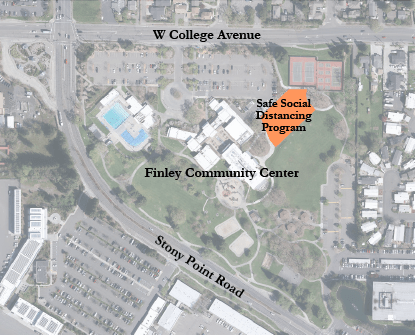
The parking lot at Finley Community Center will include up to 70 tents, spaced 12 feet apart, with each tent accommodating an individual or couple.
The tents will be provided by the city, and portable toilets, hand-washing stations, meal delivery, on-site management and services will be coordinated by Catholic Charities staff. Overnight on-site security will also be provided.
“We are moving forward with this emergency temporary measure given the urgent need to protect the City’s unsheltered homeless community as they are some of the most vulnerable to the spread of the coronavirus,” Mayor Tom Schwedhelm said in a press release. “This new, managed site offers a safer, temporary option for those who have been living outdoors in situations where social distancing is challenging if not impossible.”
Setup of the site is anticipated to begin the week of May 11, with occupancy likely beginning the week of May 18 and lasting through the duration of the county’s shelter-in-place order.
The 24,600-square-foot parking lot is located between the Person Senior Wing building and the Finley tennis courts.
More information about homeless support during the COVID-19 pandemic can be found at https://srcity.org/3284/Homelessness-Services. -
Second Coronavirus Death Reported in Sonoma County
 County health officials confirmed Friday that a second Sonoma County resident has died from complications from the coronavirus.
County health officials confirmed Friday that a second Sonoma County resident has died from complications from the coronavirus. The death was reported on the county website, socoemergency.org.
Officials have not released any further information about the person’s age, underlying health conditions or how long they had been infected, citing privacy concerns.
According to the Press Democrat, the first person to die from complications of the virus in the county was a man in his 60s with underlying health conditions who was exposed to the virus while on a cruise. County officials reported the death on March 20.
Santa Rosa police officer Marylou Armer also died from complications of the virus. She was a resident of Napa County and is not included in Sonoma County’s data. The department reported her death on Tuesday, March 31. Armer was the first Santa Rosa police officer to become infected with COVID-19.
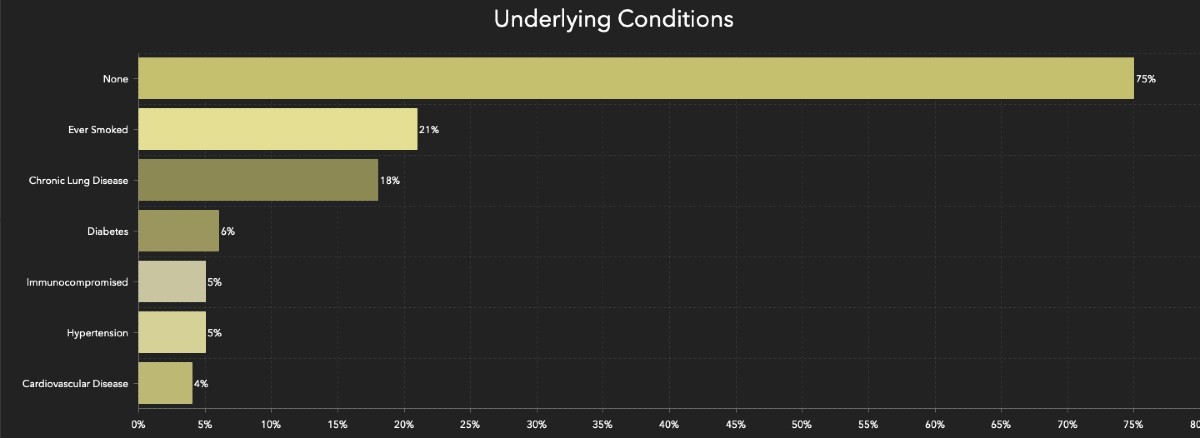
Sonoma County recently began releasing demographic data about residents infected with the virus. According to their website as of April 11, 75% of those infected in the county have no underlying health conditions. Of those diagnosed in the county, 14% have had to be hospitalized.
-
Shortage On A Stick: More Swabs On The Way, But That Won’t Solve California Test Gap
ByBen Christopher, CalMatters
 For all the talk of ventilators and new-fangled serological tests, it’s the shortage of glorified Q-tips that has brought California, the world’s fifth largest economy, to its knees. But that may be about to change.
For all the talk of ventilators and new-fangled serological tests, it’s the shortage of glorified Q-tips that has brought California, the world’s fifth largest economy, to its knees. But that may be about to change.Fresh off a phone call with President Trump, Gov. Gavin Newsom said Wednesday that the Trump administration would be sending hundreds of thousands of nasopharyngeal swabs to California in the coming weeks — providing enough to alleviate a statewide shortage of a primitive but essential coronavirus testing tool.
“We will receive just this week a minimum of 100,000 swabs. That’s the ability to collect 100,000 specimen samples,” Newsom said, adding that the feds have promised to ship a quarter-million next week and more than that in the weeks to come. “That will go a long way to give us all more confidence that we can meet some of these testing goals.”
The governor and public health experts have identified a lack of testing as one of the chief impediments to relaxing society-wide shelter-in-place orders and “reopening” the economy. Wednesday the governor also announced a goal of opening between 80 and 100 new test sites around the state before the end of the month.
(Image: Gov. Gavin Newsom said Saturday his goal is for California to acquire 10,000 ventilators. File photo by Anne Wernikoff for CalMatters)
“Testing testing testing,” Maura Calsyn, health policy director at the Center for American Progress, a center-left think tank in Washington D.C., said in a phone call last week. “In order to ‘reopen’ you have to have evidence that the rate of infection is low enough that the infection rate is not just going to spike again. And you can’t just do that blindly.”
But California’s great swab shortage is only the largest of a cascading array of supply-chain bottlenecks and resource constraints that have hampered the state’s ability to ramp up testing.
“We’ve been working seven days a week, two shifts per day,” said Christopher Catani, vice president of Hardy Diagnostics in Santa Maria, California, which produces the chemical goo used to transport test swabs to a lab while keeping any resident coronaviruses from degrading. “There are only a couple companies in the country that make that product so we’re pretty busy.”
A shortage of tests has stymied American lawmakers since the beginning of the pandemic. “Anybody that needs a test gets a test,” Trump proclaimed on March 6. It was not true then and it remains untrue.
Earlier this month, Newsom established a testing taskforce, saying that he had “a responsibility as your governor to do better.” Since then Newsom has laid out six metrics that he and his advisors will be watching.
When the state finally decides to relax its stay-at-home order will depend on progress on those metrics. “There is no date,” he said Wednesday. “If there is a date, then we’re denying the facts on the ground.”
Ramping up testing capacity is the first item on that six-part list. Newsom has set a goal of 25,000 new tests analyzed by the end of this month. At last count, he said the current number was 16,000.
But for months, suppliers have strained to meet the new demand for tests.
Nasopharyngeal swabs are necessary to collect new samples from potential patients, but they are hardly high-tech pieces of equipment. They have to be long enough to collect mucus from where the back of the throat meets the nasal cavity. They have to be flexible enough not to impale the test subject in the process. And they have to be made of a synthetic material that won’t leave behind confounding bits of cotton or wood DNA.
“Essentially it’s a little bit more sophisticated than a Q-tip,” is how President Trump put it in a press conference earlier this month.
But with only a handful of federally approved manufacturers — and one of the largest based in pandemic-ravaged northern Italy — the swab shortage has been particularly acute across the country.
“You’d think it would be easy, “said Catani of Hardy Diagnostics, which is also in the business of buying and reselling swabs. “But that’s what happens when all the manufacturers aren’t in the US.”
In Massachusetts, desperate healthcare workers have tapped engineers with 3D printers to pump out the necessary product. Last week, Parkdale-Mills, the parent company of U.S. Cotton, announced that it would begin producing a non-cotton product, the synthetic swabs. On Sunday, President Trump said he would be using the Korean War-era Defense Production Act to compel Puritan Medical Products, a manufacturer in Maine, to ramp up output for the federal government.
It is unclear where the swab shipments designated for California will come from. Asked for details, the governor’s office referred questions to the state Department of Public Health, where a spokesperson declined to specify the source of the swabs, only that they were coming from the federal government.
Newsom said that his administration conducted a survey of personnel at 251 testing sites across the state. “Fifty to 55 percent of those surveyed said that their number one need is swabs,” said the governor.
Even if officials have solved California’s swab shortage, the scarcity of tests is not over.
Early on in the pandemic, the nation was gripped by a shortfall of lab processing capacity.
That bottleneck was years in the making, said Rick Greenwood, a professor of environmental health science at UCLA and a consultant for the California Association of Public Health Lab Directors.
Since the late 1990s, more than 10 county public health labs have been shuttered or merged together across county lines.
“You get these highly trained people and particularly the smaller counties don’t want to or can’t come up with the salaries. So some of these labs closed because they couldn’t find a director,” he said. “When you lose a quarter of your capacity in your local labs, you’ve really done damage to the system.”
On March 16, the FDA relaxed some of its guidelines around the types of tests, chemical compounds and labs that can be used to analyze samples once they’re collected. That has eased pressure on labs, though some public health officials worry that in a rush to keep up with statewide testing goals, accuracy will decline.
“Everyone wants us to get back to work in the next week or month, but you have to wait for the science,” said Donna Ferguson, director of Monterey County’s public health lab. “I believe in using the most accurate tests and not using testing for testing’s sake.”
Ferrguson said that she has recently ramped up production, but only after hiring six graduate students to help with testing.
In recent weeks, capacity seems to have opened up, with industry groups of commercial labs reporting sharp drops in demand for their services — although public labs have not yet reported that decline in workload. The newfound capacity could reflect a drop off in new cases, or simply that the limiting factor is now a shortage of equipment needed to collect the samples in the first place.
“As soon as you solve for reagents, then you have to solve for RNA extraction, then you got to solve for swabs, then you’ve got to solve for viral transport, then you’ve got to solve for diagnostic timelines,” Newsom said Wednesday. “I don’t want to suggest definitively that even hundreds of thousands — even millions in the aggregate — of swabs will solve, quote-unquote, the testing issue. It will solve the swab issue.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
Sonoma County Activates “Warm Line” For Mental Health Calls
Wednesday, April 22 Update
 Sonoma County has just activated what they are calling a “Warm Line” for people to talk through any anxiety or emotional distress during the pandemic. People can call ( 707) - 565 - 2652 seven days a week from 10 a.m. to 7 p.m. Service in Spanish is available as well as interpretation for other languages.
Sonoma County has just activated what they are calling a “Warm Line” for people to talk through any anxiety or emotional distress during the pandemic. People can call ( 707) - 565 - 2652 seven days a week from 10 a.m. to 7 p.m. Service in Spanish is available as well as interpretation for other languages.At the other end of the line, counselors will offer support, guidance, and referrals.
Callers can also request a call be made to someone they are concerned about, which the county says will help to reach people who are isolated, lonely, and who may not reach out on their own.
In other news, at his daily briefing, Governor Gavin Newsom spoke about reopening hospitals to some non-emergency surgery.
Another big announcement from the governor – he’s organizing a cadre of 10,000 coronavirus contact tracers. This is a key component of the governor’s plan to reopen the state.
-
Sonoma County Allows Outdoor Dining, Summer Day Camps in Updated Health Order
 Restaurants, wineries, breweries and bars may now open in Sonoma County to serve outdoor meals.
Restaurants, wineries, breweries and bars may now open in Sonoma County to serve outdoor meals.Health Officer Dr. Sundari Mase issued an amended shelter-in-place that went into effect Saturday, May 23, that also expands childcare to include summer day-camp programs and allows drive-in ceremonies and drive-in movies. The modified order also now allows libraries to offer curbside pickup and clarifies that faith-based counseling may be delivered face-to-face when a virtual session is not possible.
A press release on the changes says that outdoor activities pose less of risk of virus transmission than indoor activities, and patrons should be limited at tables to members of the same household.
Under the order, all businesses and organizations must follow local and state guidelines for health and safety, including developing a social-distancing protocol.
The county has also developed an app called the SoCo COVID-19 Check, available in the Apple App Store and Google Play Store, that employees should be using to verify that they are healthy enough to work. Businesses have until June 1 to adopt the app.
Here’s a summary of the significant changes in this health order:
- Restaurants and food facilities may offer onsite sit-down outdoor meals
- Wineries, tasting rooms, bars, pubs, breweries and craft distilleries may offer: a) curbside pick-up, delivery, shipping; and b) sit-down outdoor meals in accordance with their land use permit and if the business has a food-facility permit (if applicable)
- Questions pertaining to food-facility or host-facility permits? Contact Environmental Health at (707) 565-6565 or
This email address is being protected from spambots. You need JavaScript enabled to view it. - Questions pertaining to land-use permits? Contact Permit Sonoma by email at
This email address is being protected from spambots. You need JavaScript enabled to view it. .
- Questions pertaining to food-facility or host-facility permits? Contact Environmental Health at (707) 565-6565 or
- Summer day camps and other educational or recreational institutions or programs may provide childcare/supervision for children of all ages
- Ceremonies (including graduations and religious activities) may be conducted with household members attending in closed motorized vehicles
-
Sonoma County Allows Retail Businesses to Offer Curbside Pick-Up, Delivery
 Sonoma County will allow nonessential retail businesses to offer curbside pick-up and delivery, and allow manufacturing and supply chain operations to function in support of approved businesses under a revised county health order.
Sonoma County will allow nonessential retail businesses to offer curbside pick-up and delivery, and allow manufacturing and supply chain operations to function in support of approved businesses under a revised county health order.The retail businesses include, but are not limited to, bookstores, jewelry stores, toy stores, clothing stores, shoe stores, home and furnishing stores, sporting goods stores, antique stores and music stores.
The updated order, effective as of Friday, May 8, coincides with the state’s move into phase two of its pandemic resilience roadmap, which allows businesses that pose a lesser COVID-19 threat to reopen.
The governor’s roadmap is comprised of four stages for reopening and criteria that counties must meet prior to entering each stage.
To accelerate further into stage two, counties must demonstrate, and public health officers attest to the state for review, that they have a low prevalence of COVID-19 spread; meet testing and contact tracing criteria; are prepared with health care system capacity to handle a sudden rise of cases; and have plans to protect vulnerable populations.
County Health Officer Dr. Sundari Mase says Sonoma County still has work to do.
“Specifically, the County needs more time to demonstrate a low prevalence of COVID-19 and no COVID-19 deaths in the last 14 days. The County is close to meeting this criteria, and will continuously review for eligibility to expand business reopening,” her health order reads.
All reopening businesses must implement social distancing and hygiene procedures based on state recommendations. In Sonoma County, businesses are encouraged to work with the Economic Development Board to develop, and begin planning to implement their protocols.
People at high risk of severe illness due to the virus are still encouraged to stay home as much as possible, and stores and shopping malls must still remain closed.
“I concur with the Governor’s assessment of our success and need for continued vigilance,” County Health Officer Dr. Sundari Mase said. “We will continually assess whether we meet the State requirements and work with the business community to make sure we are able to safely reopen additional businesses as soon as conditions and the State permit.”
Read the entire updated order and find more information at socoemergency.org.
-
Sonoma County Allows Some Businesses to Reopen
 Sonoma County has loosened some of the restrictions of its shelter-in-place order, allowing some businesses, including construction, landscaping, plant nurseries, and car and bicycle retailers, to resume operations.
Sonoma County has loosened some of the restrictions of its shelter-in-place order, allowing some businesses, including construction, landscaping, plant nurseries, and car and bicycle retailers, to resume operations.The loosening of restrictions comes as Gov. Gavin Newsom this week has approved similar reopenings for some retailers and manufacturers across the state. Health Officer Dr. Sundari Mase says the changes, which went into effect May 4, are possible because of progress in slowing the spread of COVID-19.
“Opening the County up further is contingent upon our ability to keep up our efforts and reach critical milestones,” Mase said. “Our latest data shows staying at home prevented community spread of the virus. It is important that we now work to scale up testing and contact tracing to limit the spread of COVID-19 and keep people safe.”
The revised order eases restrictions on construction businesses, real estate/rental viewing and the following essential outdoor businesses where transmission risk is lower: arborists, landscaping, gardening, pool maintenance, plant nurseries and environmental site remediation services. The order also clarifies that florists are considered essential agriculture and that their retail sales can occur only via curbside, delivery or shipping.
In addition, golfing is allowed, and automobile and bike retailers can operate.
Finally, the new order allows faith-based organizations to offer food, shelter, social services and other necessities of life for economically disadvantaged or otherwise needy individuals, and to provide counseling and host religious services through virtual streaming or similar technology.
Mase said she does not expect private or public mass gatherings to be permissible anytime soon.
The revised order does not have a specific end date, and can be amended as necessary. Mase will be working with the County Economic Development Board and industry leaders to develop specific COVID-19 mitigation measures to facilitate reopenings for all other businesses. Providing guidance to businesses is a component to move to phase two of the Governor’s Resilience Roadmap issued on April 28.
Visit SoCoEmergency.org to read the full Shelter in Place Health Order and frequently asked questions that have been developed to clarify the order.
-
Sonoma County Begins Drive-Thru Testing For Health Care Workers
By Adia White, Northern California Public MediaApril 23, 2020 On Saturday, April 25, The Sonoma County Department of Health Services Disease Control Unit will begin testing health care workers with and without symptoms. The testing will be done in the parking lot of the Public Health Laboratory in Santa Rosa. Health care workers are encouraged to make an appointment in advance by calling (707) 565-4667.
On Saturday, April 25, The Sonoma County Department of Health Services Disease Control Unit will begin testing health care workers with and without symptoms. The testing will be done in the parking lot of the Public Health Laboratory in Santa Rosa. Health care workers are encouraged to make an appointment in advance by calling (707) 565-4667.According to County Health Officer, Dr. Sundari Mase, “Being able to test our health care workers is important to keep them safe as well as our community, and ensures our health care system can continue to function throughout the COVID-19 pandemic.”
The County eventually plans to open up testing to first responders with symptoms, those over 65 with underlying health conditions with or without symptoms, and any community member with symptoms.Sonoma County recently received a shipment of medical swabs that are needed to perform coronavirus tests. These swabs have been in shortage nationwide and have limited the county's testing capacity.During a press conference on Wednesday, April 22, Dr. Mase said the County hopes to perform 200 tests a day at the public health lab. Dr. Mase is also working on forming partnerships with clinics throughout the county to further expand testing. Governor Gavin Newsom announced on Tuesday that California would need to test 60,000 - 80,000 people daily in order to reopen the state. The state is currently testing around 16,000 people each day.As of Wednesday, April 23, the County has done 4,851 tests with 4% of tests coming back positive. -
Sonoma County Human Services Department Answers Questions About Public Benefits During COVID-19
 Despite its office being closed due to the COVID-19 pandemic, the Sonoma County Human Services Department is continuing to help connect community members with public benefits.
Despite its office being closed due to the COVID-19 pandemic, the Sonoma County Human Services Department is continuing to help connect community members with public benefits.On Monday, the department shared answers to some frequently asked questions about how COVID-19 may impact public benefits such as CalFresh, General Assistance, In-Home Supportive Services (IHSS), Medi-Cal and SonomaWORKS.
“It is important to know that some state and federal reporting requirements have been adjusted to ensure that you continue to receive benefits during this difficult time,” the department said in a press release.
See their answers to commonly asked questions below. For additional information or help, email
This email address is being protected from spambots. You need JavaScript enabled to view it. or call 707-565-5800. For ongoing updates about COVID-19 in Sonoma County, visit SoCoEmergency.org.Applying for New Benefits
Q: If I need help paying for food for myself or my family, how can I apply for benefits?
A: Apply for CalFresh (a.k.a. food stamps or SNAP) online by visiting mybenefitscalwin.org or GetCalFresh.org, or apply by phone via 2-1-1. Please submit your application and required documentation, and your application interview will be waived. If you have CalFresh questions, call (877) 699-6868. For more information about the CalFresh program, please go to sonomacounty.ca.gov/Human-Services-Department.
Q: If I need cash assistance to help support my family, how can I apply for benefits?
A: SonomaWORKS (CalWORKs/TANF) provides temporary help to families with children who are having trouble making ends meet. Apply for SonomaWORKS online by visiting mybenefitscalwin.org. After you submit your application and required documentation, we will contact you to set up an application interview by phone. If you have questions about SonomaWORKS, please call (707) 565-5500. For more information about the SonomaWORKS program, visit sonomacounty.ca.gov/Human-Services-Department.
Q: I lost my health insurance or can no longer afford the cost as a result of losing my job, how can I apply for medical benefits?
A: Medi-Cal provides free or low-cost medical and dental coverage for eligible individuals and families, and has no interview requirement. To apply for Medi-Cal online, visit either mybenefitscalwin.org or coveredca.com. If you have any questions, please call (877) 699-6868.
Q: If I lost my job or had my hours reduced, how can I apply for unemployment?
A: If you have been laid off or had your scheduled hours reduced due to COVID-19, you can file an Unemployment Insurance claim online, by phone, or by mail. The Governor waived the one week waiting period for Unemployment Insurance, so you do not need to wait to apply. To file an unemployment insurance claim online, go to edd.ca.gov/Unemployment. Applying online is the best way to ensure that you get your benefits as quickly as possible. However, you can file a claim by phone: call (800) 300-5616 to apply in English or (800) 326-8937 to apply in Spanish.
Q: If I need help applying for unemployment, who can I call?
A: For limited assistance with Unemployment Insurance applications, call Job Link at (707) 565-5596. To reach the local Employment Development Department (EDD) office, email
This email address is being protected from spambots. You need JavaScript enabled to view it. or call (707) 576-2850. Please leave a specific voicemail message and a staff member will respond to your call as soon as possible.Renewing Your Existing Benefits
Q: Do I need to call or visit a Human Services Department office to renew my CalFresh, General Assistance, or SonomaWORKS (CalWORKs) benefits?
A: You do not need to call nor visit one of our offices to renew your CalFresh, General Assistance, or SonomaWORKS (CalWORKs) benefits at this time. Current recipients will continue to get benefits at the same level (without interruption) for March, April, and May 2020. If you had a recertification due in March, April, or May 2020, expect to receive a letter saying that your recertification will be due six months from your original due date. For example, if your original recertification was due in March 2020, it will now be due in September 2020. This applies to both annual recertification and periodic reports (Semi-Annual Report, a.k.a. SAR 7). Regular reporting requirements for CalFresh, General Assistance, and SonomaWORKS are expected to resume in June 2020.
Q: Will I be required to complete my work requirements during the COVID-19 crisis?
A: The work requirements for General Assistance and SonomaWORKS (CalWORKs) Welfare-to-Work have been waived for the months of March, April, and May 2020. If you are still able to complete your assigned activities, please turn in your attendance as usual. However, if you are unable to submit attendance during the COVID-19 crisis, you will not be penalized.
Q: What is a CalFresh Emergency Allotment?
A: The CalFresh Emergency Allotment is an increase to your benefits that will be automatically added to your EBT card for March and April 2020. The allotment will increase CalFresh benefits to the maximum amount for eligible household members (up to six individuals). You can expect the first allotment (for March) to be added to your EBT card on April 12th and the second allotment (for April) to be added on May 10th, 2020. If your household is already receiving the maximum amount for CalFresh, no additional benefits will be issued.
Q: If I lose my EBT card, can I still get it replaced?
A: Please call the customer service number at (877) 328-9677 to request a replacement EBT card. If you require an emergency replacement: CalFresh recipients can visit 2550 Paulin Drive in Santa Rosa and SonomaWORKS recipients can visit 2227 Capricorn Way, Suite 100, in Santa Rosa. The lobby doors will be locked; however, our reception staff will be available Monday - Friday between 8:00am - 4:30pm to assist you with this type of critical need. To protect yourself and others, we ask that you wear a face covering, wash your hands, and respect social distancing guidelines.
Q: If I lose my Medi-Cal Identification Card (BIC), can I still get it replaced?
A: Yes, please contact our service center at (877) 699-6868 to request a new Medi-Cal Identification Card (BIC). If you need to access services right away, most Medi-Cal providers can confirm your eligibility in their office by using your social security number.
Q: What can I do if my children are currently covered by a Medi-Cal program with a monthly premium that I cannot afford as a result of COVID-19?
A: If your children receive health care coverage through the Medi-Cal For Families program and you cannot pay the premium due to COVID-19, you can request a waiver of your premium by calling the Medi-Cal For Families Payment Section at (800) 880-5305.
Q: Do I need to call or visit a Human Services Department office to renew my Medi-Cal benefits?
A: No. Due to the Governor’s executive order, current Medi-Cal recipients will continue to receive benefits for March, April, and May 2020. All negative actions have been delayed for Medi-Cal beneficiaries and will be processed at a later date. If you receive information from the county, including renewal packets for Medi-Cal, please make sure to respond. Renewals can be returned via mail or uploaded via mybenefitscalwin.org.
Q: Will In-Home Supportive Services (IHSS) be impacted by COVID-19?
A: In-Home Supportive Services (IHSS) continues to provide services remotely. IHSS referrals can be made through the regular process of calling (707) 565-5900. IHSS social workers are working remotely and able to respond to calls, do outreach to vulnerable clients, and complete assessments by phone. Note that the state still currently requires an in-person interview for new IHSS applications, which will be completed once it is safe to do so.
Q: Does COVID-19 affect In-Home Supportive Services (IHSS) Payroll or Public Authority?
A: In-Home Supportive Services (IHSS) Payroll and Public Authority are providing all services, including supporting new provider enrollment and referring new providers to clients. Please call (707) 565-2852 for IHSS Payroll and (707) 565-5700 for IHSS Public Authority.
Reporting Abuse or Neglect
Q: How can I report concerns about child abuse or neglect?
A: If a child is in immediate danger, call 9-1-1 right away. Otherwise, please call the confidential Child Protection Hotline at (707) 565-4304 or (800) 870-7064 to report your concerns regarding child neglect, parental abandonment, and emotional, physical, or sexual abuse.
Q: How can I report abuse or neglect concerns about an older adult or dependent adult?
A: If you are concerned that an older adult (age 60+) or dependent adult (age 18+) may be experiencing neglect or emotional, physical, financial, or sexual abuse, please call the confidential Adult Protective Services (APS) Hotline at (707) 565-5940 or (800) 667-0404.
-
Sonoma County Library Sees Dramatic Spike in Digital Circulation, Use of Online Resources During Pandemic
 At the Sonoma County Library, the shift from physical books and resources to digital ones has been slow but steady over the past few years.
At the Sonoma County Library, the shift from physical books and resources to digital ones has been slow but steady over the past few years.“Every year, we see more and more patrons checking out electronic books, streaming movies, tracing their family tree or conducting research,” Library Director Ann Hammond said in a press release. “Some of our most loyal and active patrons rarely come into a branch.”
But since closing all of its branches due to the coronavirus pandemic and county shelter-in-place orders on March 14, the library reports a dramatic spike in its digital circulation numbers.
OverDrive, a popular way to check out electronic books and audiobooks through the library, had a 356 percent increase in use from March 17 to April 8. In the same period, the library’s Hoopla platform, which offers books, films, TV, music, comics and more, had a 786 percent increase.
Kanopy, a resource for classic films and documentaries, had a 298 percent increase, and RBDigital, which connects readers with thousands of current issues and back issues of magazines, saw the largest jump with a 2,434 percent increase in use.
The library says patrons are discovering all of the digital resources available to them for free with a library card — enabling them to do things like learn languages with Mango, brush up on software skills with Lynda, decide what home appliance to purchase with Consumer Reports, research car repairs with Chilton, look up ancestors on Ancestry.com, or read the New York Times.
And Hammond doesn’t think the shift to digital will be temporary.
“There is no substitute for a one-on-one conversation with a friendly librarian, or attending a library event, or bringing your child to a story time, but a lot of our patrons are discovering how easy it is to try the digital option, and we’ll be prepared to keep supporting them,” she said. “We’ve already added or expanded digital resources, and we will keep looking for ways to serve our community, in person or online.”
One enduring concern, however, is that not everyone has access to the Internet.
“We have free high speed WiFi in our branches, and it’s still on during the closures so people can access it from outside when the building structure permits,” Hammond said. “We also have more than 500 WiFi hotspots and more than 100 Chromebooks in circulation, but it’s not nearly enough.”
Hammond says when branches eventually reopen, the library will continue to advocate on behalf of those who can’t afford broadband.
“This is a wake-up call for every library in America,” she said. “We can’t close the digital divide by ourselves, but we intend to be loud and persistent voices in finding a solution.”
-
Sonoma County Medical Facilities Must Screen Staff, Visitors for COVID-19 Symptoms and Require Masks
 Sonoma County’s health officer has issued a new order requiring all congregate care facilities to screen all staff and visitors for signs of illness and adhere to a strict mask-wearing policy to slow the spread of COVID-19.
Sonoma County’s health officer has issued a new order requiring all congregate care facilities to screen all staff and visitors for signs of illness and adhere to a strict mask-wearing policy to slow the spread of COVID-19. The order, which went into effect April 17, applies to all medical care facilities, licensed residential care facilities, including nursing and senior care facilities, psychiatric facilities, group homes, residential recovery houses and homeless shelters.
The order stipulates that before starting work, all staff in congregate settings and first responders must perform a symptom screen and have their temperature taken.
(Image: Sailors assigned to the hospital ship USNS Mercy admit a patient in Los Angeles, March 29, 2020. Credit: US Nacy)
Anyone who is not a patient or resident at a patient care facility must wear a medical-grade isolation or surgical mask at all times while in the facility, and submit to a temperature and symptom screening upon entry.
“It’s critical that we do all we can to protect our first responders, medically vulnerable patients, and people who must be cared for outside the home in congregate settings,” said Susan Gorin, chair of the Board of Supervisors. “This country has already witnessed how quickly the virus can spread in these settings.”
Non-clinical facilities that provide overnight care and day services have the option of requiring staff and visitors to wear fabric or cloth face coverings instead of medical-grade masks.
Additional requirements for patient care facilities include social distancing in meal and break rooms, and avoiding the use of employees or staff who have worked at another facility within the past 14 days.
The order defines first responders as those who provide 24/7 emergency response, first aid care, or other related assistance either in the course of the person’s occupational duties or as a volunteer, such as peace officers, emergency medical technicians, firefighters, rescue workers, certain social workers and certain animal control officers.
Visit SoCoEmergency.org to read the order or for more information about COVID-19.
-
Sonoma County Offers Expanded Drive-Thru COVID-19 Testing for Vulnerable Individuals
 Additional groups of high-risk and vulnerable people will now be able to get tested for COVID-19 at Sonoma County’s drive-thru testing site at the county’s Public Health Laboratory.
Additional groups of high-risk and vulnerable people will now be able to get tested for COVID-19 at Sonoma County’s drive-thru testing site at the county’s Public Health Laboratory.The site, operated by the Department of Health Services (DHS) Disease Control Unit, will now be available to the following groups:
- Health care workers (with or without symptoms)
- First responders (with or without symptoms)
- First responders include people who provide 24/7 emergency response, first aid care, or other related assistance either in the course of the person’s occupational duties or as a volunteer and include:
- Police officers
- Firefighters
- Paramedics and EMTs
- Emergency Response Social Workers
- First responders include people who provide 24/7 emergency response, first aid care, or other related assistance either in the course of the person’s occupational duties or as a volunteer and include:
- Symptomatic people over 65 years of age
- Symptomatic people with underlying health conditions
- All essential workers (with or without symptoms)
- Examples of essential workers include:
- grocery store workers,
- In-Home Supportive Services (IHSS) caregivers,
- construction workers,
- utility workers
- childcare providers,
- or anyone who has continued to work under the Shelter in Place health order in an essential function.
- Examples of essential workers include:
The tests are free and available by appointment only by calling (707) 565-4667. The testing site is located at 3313 Chanate Road in Santa Rosa.
The other options for testing in Sonoma County are:
- State testing sites:
Testing is available at sites operated by OptumServe, a health services contractor for the State of California. Testing locations are in Santa Rosa and Petaluma. Appointments can be made online at https://lhi.care/covidtesting. People without internet access or who need to make an appointment in a language other than English can call 1-888-634-1123. Information and frequently asked questions are available at socomergency.org/sonoma-county-increases-covid-19-testing-with-two-new-community-testing-sites/. - Through your medical provider:
Individuals with coronavirus symptoms should still contact their medical providers to seek treatment and testing.
All tests are free and available regardless of immigration status. There is currently no coronavirus antibodies test.
“Community-wide testing is a critical step toward re-opening the County,” said Dr. Sundari Mase, county health officer. “Expanded testing allows us to identify and increase our understanding of COVID-19 community spread. This includes collecting a broad sample of results, including data from those in specific groups and those who do not have symptoms. Upwards of 30% of people who test positive experience no symptoms, but can still spread the disease.”
Find the latest updates regarding the coronavirus emergency, local resources and other helpful information at SoCoEmergency.org. -
Sonoma County Submits Plan to State for Reopening More Businesses, Including Outdoor Bar, Restaurant Patios
 Sonoma County’s health officer has submitted a plan to the state asking for approval to move further into Stage Two of reopening the local economy, including allowing outdoor bar and restaurant patios to open.
Sonoma County’s health officer has submitted a plan to the state asking for approval to move further into Stage Two of reopening the local economy, including allowing outdoor bar and restaurant patios to open. The request follows the California Department of Public Health’s announcement Monday of a new “attestation opportunity” for counties to affirm to the state that they have met certain COVID-19 health and safety measures allowing them to open additional businesses at their own pace. The updated requirements include stable or declining hospitalization rates, testing and contact tracing capacity, and plans for containing outbreaks.
“Anticipating the need and appropriateness of allowing additional counties to control the focus of restrictions for their own jurisdictions, state public health leaders are now creating opportunities for additional counties to assume more local control in Stage 2 and improve local level preparedness,” a CDPH press release reads.
The county Board of Supervisors had unanimously approved early on Monday the attestation put together by Health Officer Dr. Sundari Mase. At noon, Gov. Gavin Newsom announced amended criteria that Supervisor James Gore said pushed Sonoma County’s metrics even further “into the green.”
Mase said she believes there could be a new county health order as soon as Friday, once the state approves the attestation. Sonoma County’s plan does not include indoor dining or shopping centers.
Some labor groups, including health care workers, oppose further reopening the local economy. A press conference by North Bay health care professionals on Tuesday planned to discuss some of their concerns.
"Healthcare professionals in Sonoma County have grave concerns about the readiness of our county to re-open due to continued significant risks of COVID-19. Our main concerns are inadequate PPE, testing capacity definitions, isolation support, and lack of health equity focus," the media invitation reads.
As of Monday, 24 mostly rural counties had received permission from the state to reopen restaurants and shopping centers, with modifications. The counties make up roughly 5% of the state’s total population.
Higher-risk workplaces and gatherings, including nail salons and movie theaters, are not being approved by the state for reopening at this time.
-
Sonoma County To Establish Surge Hospital At Sonoma State University
 Sonoma County is establishing an alternative care site (ACS) at Sonoma State University where about 580 patients can be treated in the event of a COVID-19 surge.
Sonoma County is establishing an alternative care site (ACS) at Sonoma State University where about 580 patients can be treated in the event of a COVID-19 surge.The site will be operated by the Petaluma Health Center, and patients will be placed in the Recreation Center and in a portion of the residential housing area on the SSU campus.
The county has been using COVID-19 modeling data to inform the development of an ACS to support local hospitals and has been working with health care providers and partners to identify the types of patients that might seek care, and facilities that might be needed. SSU was selected from a number of sites.
“We're grateful to Sonoma State for filling such an important role," said Susan Gorin, chair of the Board of Supervisors. "Having alternate care sites will be crucial if our hospitals experience a surge in patients. We hope we won't be in that situation, but it's imperative we plan for it and have resources ready."
The gymnasiums in the Recreation Center will be used for COVID-19-positive patients with mild-to-moderate symptoms, while the residential units will be used for those who are awaiting test results for COVID-19. A separate residential housing complex will be used for COVID-19 vulnerable individuals — those who are over the age of 65 and those with underlying medical conditions. The county said capacity at the site can be increased if necessary.
State Sen. Mike McGuire, who represents a significant portion of the county, was a proponent of having an ACS at SSU.
"This is a historic, all-hands-on-deck effort to expand our hospital capacity across this state and here at home in Sonoma County,” he said. “Opening up these over 500 beds will be a huge boost to expanding our local surge capacity. We are truly grateful for the one hundred percent partnership between Sonoma State University and the County of Sonoma — we know there’s much more work ahead.”
-
State Dashboard Tracks Daily COVID-19 Hospitalizations By County
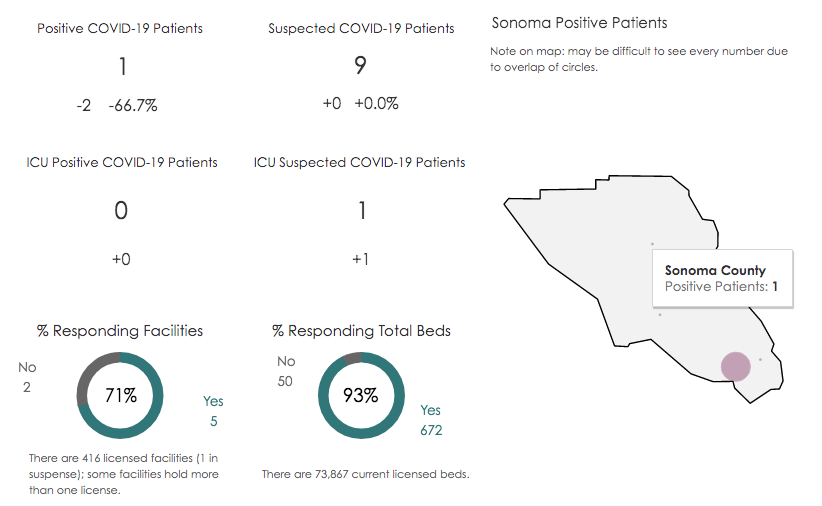 On April 1, the California Department of Public Health released a data dashboard that tracks coronavirus hospitalizations by county.
On April 1, the California Department of Public Health released a data dashboard that tracks coronavirus hospitalizations by county. The dashboard shows the number of hospitalizations reported each day in connection with the virus. Patients are listed in four categories: hospitalized patients who have tested positive for the virus, hospitalized patients suspected of having the virus due to exhibiting symptoms typically found in COVID-19, patients in intensive care who tested positive for the virus, and patients in intensive care suspected of having the virus.
In Sonoma County as of April 28, with 71% of hospitals (93% of licensed beds) reporting to the state, there are 9 suspected COVID-19 patients and 1 positive patient.
-
Tips for Spotting Fake News Stories — And Where to Find Sources You Can Trust
 Anytime there’s a significant news event — like a global pandemic, for example — you can expect misinformation to spread across the Internet.
Anytime there’s a significant news event — like a global pandemic, for example — you can expect misinformation to spread across the Internet. “Fake news” means stories that contain fabricated information, or information that’s based on rumor, shoddy methodology or a partisan agenda.
With the coronavirus, popular fake news stories have included reports that the virus is a manmade bioweapon and that it can be cured by eating garlic or high doses of Vitamin C, among many others.
A Pew Research Center study found that about half of U.S. adults (48%) report having come across at least some news and information about COVID-19 that seemed completely made up, with 12% saying they have seen a lot of it and 35% saying they have seen some.
In light of the prevalence of these dubious stories, we wanted to share some tips for identifying fake news and finding information you can trust.
Spotting Fake Stories
Tip 1: Check the source
Click away from the story to look into who the publisher is, read the site’s “About Us” page or mission statement, check the domain name (be wary of unusual top-level domain names, like “.com.co.), investigate who the author is and what else they’ve published. Does everything seem credible, real and trustworthy?
Tip 2: Read beyond the headline
Headlines can be misleading — often written with sensational claims to get clicks. What’s the whole story? If the story seems outlandish, make sure it’s not a piece of satire.
Tip 3: Pay attention to quality and date
Spelling errors and dramatic capitalization don’t fly at credible news outlets. Also, check when the story was published. Re-publishing old stories can take information out of context.
Tip 4: Check the sources and citations
Credible journalism is led by gathering facts from people, documents and other publications, which means you should see quoted material in the story with named sources and links, when relevant, to information that supports what’s written. If you came across the story on social media, make sure to click through to the story and investigate the publisher as outlined in Tip 1. You can’t always trust what’s shared by your friends.
Tip 5: Check your biases
Does the story tell you what you want to hear? Does it only confirm what you already suspected? Consider if your own beliefs could affect your judgment.
Tip 6: Consult professional fact-checkers or experts
There are many websites dedicated to debunking false information online. Google the topic + fact check, ask a librarian, or do your own detective work to determine fact from fiction.
COVID-19 Sources to Trust
When it comes to the current coronavirus pandemic, the best places to turn to for reliable, trustworthy information are public health organizations and officials, your local and state government, and nonprofit news organizations.
Locally, you can look to your county and its Department of Public Health or Office of Emergency Services for updates and resources. (In Sonoma County, that would be https://socoemergency.org/.)
For state information, look to the Governor’s Office or state Department of Public Health. California Gov. Gavin Newsom has been holding daily briefings on the crisis most days at noon (look to his Twitter page for announcements), and the CDPH is keeping track of case count totals and providing other resources.
Federal organizations to turn to for factual health information include the Centers for Disease Control and Prevention and the World Health Organization.
Local news organizations (like NorCal Public Media!) are also great places to turn to for the latest news and context.
Above all, it’s important when consuming the news to maintain curiosity, be reflective about what you’re reading, actively investigate your sources and look for in-depth coverage. Take breaks when you need to — there’s way more information out there than is necessary for you to stay safe and healthy.
Citations for this story include:
Cornell University
Harvard University
Pew Research Center
NewsGuard -
Track County COVID-19 Cases, Hospitalizations and Deaths

As COVID-19 continues to spread across the nation, understanding the pandemic’s effect on your local area can be difficult.
That’s why four public media organizations have collaborated to create the California COVID-19 Tracker — a data dashboard that provides a localized look at COVID-19-related cases and deaths in each county, as well as a risk assessment for each county’s population.
The tracker also looks at how many people in each county are at high risk for a severe case of the disease by showing how many residents are 65 and older, suffer from chronic respiratory disease, cardiovascular disease and diabetes.
Case and death data is collected by hand by reporters for CapRadio, KQED and KPCC from each public health department or county’s individual site each evening. They update the data daily at 7 or 8 p.m, and many jurisdictions post in the late afternoon.
Track county hospitalizations and skilled nursing facility caseson the California Department of Public Health website.
This dashboard was created by Allie Kanik at Louisville Public Media, Lisa Pickoff-White at KQED, Emily Zentner at CapRadio and Dana Amihere at KPCC.
-
Two COVID-19 Testing Sites Will Open for Residents With and Without Symptoms
By Adia White, Northern California Public MediaUpdated May 3, 2020 Sonoma County is launching two new coronavirus testing sites in Santa Rosa and Petaluma that will be open to community members with and without symptoms. The sites will open on Tuesday, May 5, and are provided through the State of California in partnership with the private company, OptumServe.Tests are available by appointment only. To make an appointment call 1-888-634-1123 or visit https://lhi.care/covidtesting. According to a press releasesent out by the County of Sonoma, tests will be available for free for community members without insurance. Insurance companies will be billed for all other tests.(Image: COVID-19 test kits. Credit: The Centers for Disease Control and Prevention.)
Sonoma County is launching two new coronavirus testing sites in Santa Rosa and Petaluma that will be open to community members with and without symptoms. The sites will open on Tuesday, May 5, and are provided through the State of California in partnership with the private company, OptumServe.Tests are available by appointment only. To make an appointment call 1-888-634-1123 or visit https://lhi.care/covidtesting. According to a press releasesent out by the County of Sonoma, tests will be available for free for community members without insurance. Insurance companies will be billed for all other tests.(Image: COVID-19 test kits. Credit: The Centers for Disease Control and Prevention.)
The two new testing sites in Sonoma County are a part of Governor Gavin Newsom's plan to expand testing capacity statewide. On April 22, Governor Newsom announced his office would launch at least 80 new testing sites across the state. These sites will increase the state's testing capacity by more than 10,500 tests per day and the County's testing capacity by more than 260 tests per day.In a press release, Board Chair Susan Gorin said that “This will help us get reach our goal of conducting 600 - 800 tests per day, which will help us to understand the spread of COVID-19 here in Sonoma County – a critical step toward opening the County back up.”Increased testing capacity is one of six criteria that Governor Gavin Newsom said will drive the state's decision to lift shelter in place. Other criteria include preventing infection in people who are most at risk, being able to handle surges in hospitals, developing therapeutics to meet demand, ensuring businesses, schools, and child care facilities can support physical distancing, and setting criteria as to when to reinstate the stay-at-home order if need be. -
Undocumented Workers Face Obstacles Qualifying for Benefits During the Pandemic
By Jacqueline Garcia, La Opinión and Erica Hellerstein, Mercury News
 Before the COVID-19 pandemic, Hector had a stable job as a cook at an Italian restaurant in Oakland. Suddenly, in mid-March, about a dozen workers were laid off, including him.
Before the COVID-19 pandemic, Hector had a stable job as a cook at an Italian restaurant in Oakland. Suddenly, in mid-March, about a dozen workers were laid off, including him.“There was a low clientele and the restaurant wasn’t doing well,” said Hector, who didn’t want to provide his last name due to his undocumented status.
Hector, a 45-year-old married father of three and a grandfather, was left struggling to care for his family. Because he is undocumented, he does not qualify for unemployment insurance.
Yet many undocumented workers are unaware that they can apply for other state benefits that are available to out-of-work employees.
(Image: Legal Aid at Work attorney Kim Oulliette assists a client. Photo courtesy of Legal Aid at Work)
Hector recently found out that he may qualify for disability insurance payments when he visited a local health clinic to take care of a painful ingrown toenail and other health issues. Since a car accident two years ago, “I suffer from a lot of headaches, my arm and my hand hurt a lot, too,” said Hector, a native of Mexico.
His doctor said that due to his multiple health problems, he might qualify, so he is in the process of applying.
“I hope I do get approved because in every paycheck we get deducted an amount of money [for disability] and when the government does that, they don’t ask us if we have papers or not,” said Hector. “The small amount of savings we had is disappearing.”
Many advocates and service providers say the coronavirus and stay-at-home orders have had a disproportionately high impact on undocumented and low-wage workers.
Undocumented workers who lost their job during the pandemic because they are sick, quarantined or ordered to stay at home because of chronic conditions don’t qualify for unemployment. But they can qualify for state disability insurance, paid family leave and workers compensation.
There are many obstacles however: The only way to fill out the application without a Social Security number is to submit a paper application. Plus, they need a doctor’s authorization, while many undocumented workers are uninsured and can’t afford doctors.
Alexis M. Alvarez, a senior staff attorney at the San Francisco-based nonprofit Legal Aid at Work, is advising Hector with his process of applying for disability payments.
“Both of those benefits, paid family leave and state disability insurance, your citizenship and immigration status doesn’t matter because they don’t require you to be able and available to work in the same way that unemployment insurance does,” said Alvarez.
Undocumented workers may qualify for family leave when they need to leave work to care for a family member with an illness or disability.
In both cases, they have to provide a doctor’s note.
California is home to more than 2 million undocumented immigrants, making up nearly 1 in 10 workers in the state. About two-thirds have resided in the state for longer than 10 years, according to the Public Policy Institute of California.
Many are taxpayers. In 2014 undocumented immigrants in California paid about $3.2 billion in state and local taxes.
In addition, like all workers, undocumented employees have money deducted from each paycheck to pay for disability insurance.
Alvarez said whether it is state disability insurance or family leave, the worker doesn’t need a Social Security number or Individual Taxpayer Identification Number (ITIN). But they must provide proof of income like a W-2.
To apply, workers must apply on paper and leave the spot blank asking for a Social Security number. Alvarez said the response takes two to three weeks.
The application can be obtained from the state Employment Development Department through its website. “The other couple of places where I know you know people can get copies, if there are some, is through community organizations, medical offices or other nonprofits like ours that keep paper copies in their offices,” said Alvarez.
However, with social distancing, many of these places are closed to the public, leaving affected employees few options.
In addition, language problems or lack of experience using a computer are other barriers that stop undocumented workers from applying.
Worker’s comp also available
California Insurance Commissioner Ricardo Lara recently announced that workers sickened by COVID-19 are eligible for workers’ compensation benefits regardless of their immigration status. This includes workers engaged in front-line occupations such as health care, emergency services, food production, sales and delivery, among others.
“This unprecedented pandemic has sparked questions and concerns among essential workers in the immigrant community who are showing up for work every day, bringing us vital goods and services,” Lara said in a statement. “Hardworking Californians who are exposed to COVID-19 are entitled to workers’ compensation benefits if they fall ill, regardless of their immigration status.”
But the reality is that most workers affected by the crisis are not eligible because the funds are for people who are sick, said Kim Oulliete, an attorney with Legal Aid at Work.
“And the vast majority of people right now have just been laid off,” she said. “And where the state has been directing most people for assistance is unemployment insurance, but undocumented cannot apply.”
Advocating for the most vulnerable
Legal Aid at Work united with a coalition of more than 100 organizations to urge Governor Gavin Newsom to create a “Disaster Relief Fund” to help undocumented immigrants until the state’s emergency proclamation is lifted and people return to work.
“Already, undocumented immigrants are living precariously—over half live at or below 150% of the poverty level,” the letter says. “Accordingly, it is imperative that the state meet these workers’ basic needs so that they can comply with the Shelter in Place Order without fearing that they will not be able to feed and house their families.”
Members of the state’s Latino Legislative Caucus have called on Newsom to extend the California Earned Income Tax Credit to undocumented workers who file taxes with an ITIN number and provide MediCal benefits to all low-income undocumented adults.
Newsom recently signaled that the legislature is working on a relief package for undocumented immigrants but did not provide specifics about the plan.
“California cares deeply about undocumented residents in this state,” Newsom said.
Maria Hernandez, a 44-year-old housecleaner, hasn’t had work since the Bay Area implemented the nation’s first shelter-in-place order in mid-March.
“I can’t apply for many resources and this gives me so much anxiety,” Hernandez says. “We are only one family and there are tons of families that are suffering in those moment for being undocumented, and there is a lot of fear to ask for help because of the fear of being deported, of losing housing. My community is very vulnerable.”
As pressure mounts on state and federal officials to support the taxpaying undocumented workforce, new local resources are popping up to help people.
In the Bay Area, financial assistance programs for undocumented workers affected by COVID-19 related job losses have sprung up in San Francisco, Sonoma County, and Oakland. A relief fund for local migrant youth affected by the state’s shelter-in-place order was launched in Santa Clara, San Mateo, Contra Costa, Marin, San Francisco and Alameda counties, but is no longer taking applications.
“As soon as the Bay Area issued its shelter-at-home orders we started getting calls from folks who were losing their work or wondering about whether they had to go to work because it felt all of a sudden very unsafe,” said Derek Schoonmaker, an attorney at the Oakland-based Centro Legal de la Raza, which recently launched a relief fund for undocumented Oakland workers who have lost jobs or income.
“The clients we work with are often paycheck to paycheck. They are depending on their week’s paycheck to cover basic needs like rent and food, so taking a hit in their income can mean a real scramble to get that together to meet those needs.”
In the past several weeks, Schoonmaker said, the fund has raised roughly $330,000 — primarily from a grant from the City of Oakland, foundations, and individual donors — and has received more than 1,500 applications from undocumented workers. The fund will distribute $500 grants to each applicant, but so far can’t help everyone who applied due to the volume of applications.
In addition, teachers and administrators in the Oakland Unified School District have launched a program where people can turn over their federal stimulus checks to undocumented families.
Yet some of the groups administering grants say their efforts will have a limited impact without broader policy changes.
Across the U.S., immigrant’s rights groups, labor organizations and some lawmakers are calling on national officials to provide relief for undocumented workers ineligible for food and other safety net benefits and left out of the federal government’s coronavirus stimulus checks, with a particular focus on those workers who filed taxes with ITINs.
“The relief checks ignore the contribution of immigrant families and the essential contribution they are making now and missing the fact that they are families that have been paying into the system and contributing in a formal way to our economy,” said Erin Quinn, senior staff attorney at the Bay Area-based Immigrant Legal Resource Center.
Congressman Lou Correa (D-CA) has introduced the Leave No Taxpayer Behind Act, which would ensure that immigrants who filed taxes with ITIN numbers would be eligible for the government’s $1,200 coronavirus relief check.
Jacqueline García is a reporter with La Opinión and Erica Hellerstein is a reporter with the Mercury News. This article is part of The California Divide, a collaboration among newsrooms examining income inequity and economic survival in California.
-
Wear a Mask! OK, But What Kind?
 ByJulie Cart, CalMatters
ByJulie Cart, CalMattersThe Centers for Disease Control and Prevention on Friday recommended every American wear a face mask while in public to protect against contracting coronavirus.
The agency announced that non-medical fabric masks – even scarves or bandannas – could help slow the spread of the infection. State health officials earlier in the week made the same recommendation.
The ever-evolving response to the coronavirus pandemic has amped up the need for keeping everyone safe from the virus.
That means wearing masks.
(Image: Food bank volunteer Betty Kimmel wears a protective mask as she hands out oranges to seniors at Teamsters 315 Hall in Martinez on March 19, 2020. Photo by Anne Wernikoff for CalMatters)
What is the purpose of a face mask?
It depends on who is wearing it.
Humans have long covered their faces to ward off disease, and medical masks have a long and colorful history .
For most of the public and some healthcare workers, “the main purpose of a mask is not to protect yourself from others, but to protect others from you,” said Bill Padula, an assistant professor at the University of Southern California’s School of Pharmacy.
Padula, who studies patient and worker safety in hospitals, said medical masks are designed to protect the wearer from contact with an infected patient.
“It isn’t simply thinking about what I have to do for this patient sitting in front of me, but ‘How do I treat this patient, with respect to the next 10 patients who walk into this clinic?’” he said.
In its new guidelines set Friday, the CDC said studies have shown that “a significant portion” of people with the virus have no symptoms and can still spread the virus. “In light of this new evidence, CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.”
Which masks are in short supply?
The highly-contagious coronavirus requires doctors, nurses and other clinicians to take extra precautions when treating patients. With more than 1 million people worldwide infected, there is a critical shortage of N95 masks and surgical masks — the types worn by healthcare providers.
The N95 respirator mask is a polymer cup designed to fit snugly to the face to form a seal, and filters out nearly 95% of airborne particles. The federal government suggests they not be reused or shared.
In contrast, surgical masks are made with multi-layered fabric, commonly pleated, with bands that hook over ears, and are worn loosely. They are designed to provide a physical barrier that prevents the spread of germs from person to person.
They also are not intended to be used more than once.
But in both cases, hospital officials in hard-hit cities such as New York have rationed the masks and are washing and reusing them.
The situation is made worse by the fact that about half of the world’s supply of medical masks is manufactured in China, with many of the factories located in Wuhan, thought to be the epicenter of the coronavirus outbreak.
What about other types of masks, will they work?
In many fire-prone communities around California, homeowners and local community emergency agencies maintain stocks of masks intended to protect the wearer from wildfire smoke.
Some of these are known as P95 masks, often recommended by fire officials for use by residents during wildfires. The masks — sometimes referred to as dust masks — are fitted with a small carbon filter, designed to protect against oil-based particles.
They work well in many applications, but are not considered medical-grade masks and are “not commensurate with current U.S. standards of care,” according to the Centers for Disease Control and Prevention.
Federal guidelines go on to say, however, that P95 masks, alone or in combination with other measures, are acceptable when there are shortages of N95 respirators. “These devices are expected to be suitable alternatives to provide protection during the COVID-19 response when supplies are short,” the CDC guidelines say.
The guidelines do not say why P95 masks, which block the same percentage of particles as the others, do not meet federal standards for health care workers. It is likely that they have not been fully studied to ensure that their filtration ability, seal and other factors meet the needs of hospitals, since they were not designed for that use.
How about donating those wildfire masks to hospitals and local clinics?
Napa City Council Member Liz Alessio organized a local donation drive that gleaned some 45,000 masks, the bulk of them surgical masks but some from people’s stocks of P95 masks.
The region’s vulnerability to wildfire meant that “folks had masks in their homes and businesses,” Allesio said. “There’s a lot more out there.”
Health care officials are most appreciative.
“We are humbled by the outpouring of support we have received from our communities and business partners to help source additional supplies,” healthcare HMO Kaiser Permanente said in a statement to CalMatters.
But the company said it was organizing a donation network and discouraged people from bringing donations directly to medical centers.
The California Department of Public Health told CalMatters that while the P95 fire masks are “highly effective,” it is “up to the individual medical institution to decide if they are acceptable for use by personnel.”
At least one hospital told Allesio that it would not be able to use the donated P95 masks because they didn’t meet the hospital’s requirements.
Medical masks are regulated by the Centers for Disease Control and Prevention, the National Institute for Occupational Safety and Health and the federal Occupational Safety and Health Administration.
The state launched a website where individuals and companies can donate or sell scarce medical supplies, including masks. The site specifically mentions N95 and surgical masks only.
Ok, what are the rest of us supposed to do?
Before this week, officials downplayed the need for most people to wear masks when they are out in public, provided they practice appropriate physical distancing. Then, as it became more clear that there are unknown numbers of asymptomatic people officials are now urging everyone to use face coverings, as well as remain at least six feet apart.
There is a wide variety and many gradations of face masks anyone can use, including rudimentary paper dust masks, often used for home DIY projects.
Barbara Ferrer, director of the Los Angeles County Public Health Department, said that for most people, a homemade mask using tightly woven cotton fabric, a bandanna or scarf affords sufficient protection.
“There really is no need for anyone in the public to go and secure N95 masks, I beg you not to,” she said. “They are needed by medical workers or health care workers.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
What Comes Next for California Cities? Deficits, Bailouts and Long Recoveries
ByJackie Botts,Ben Christopher,Elizabeth Castillo,Ana B. Ibarra andMatt Levin, CalMatters
 Cities have been ground zero in California’s coronavirus response — with many initiating shelter-in-place orders, organizing emergency housing for homeless people and supporting health and essential workers. But even before restrictions get lifted, mayors, managers and city councils are being tested in a new way: pandemic-induced budget deficits.
Cities have been ground zero in California’s coronavirus response — with many initiating shelter-in-place orders, organizing emergency housing for homeless people and supporting health and essential workers. But even before restrictions get lifted, mayors, managers and city councils are being tested in a new way: pandemic-induced budget deficits. Already, unemployment is projected to be higher than it was during the Great Recession. Sales and property tax revenues have cratered. And while some of a $150 billion Coronavirus Relief Fund tucked into the federal stimulus CARES Act will go directly to large cities with a population of 500,000 or more, the League of California Cities has already declared it insufficient.
Across California cities, the clamor for a federal bailout is growing. Whatever reserve they may have built up during the recovery is being wiped out and replaced by red ink. City hall leaders now face an unsavory menu of service cuts, furloughs and staff reductions. Public employee pension and health care obligations will only add to the pain.
(Image: A woman pushes a cart past the shuttered Fox Theater in downtown Oakland on March 25, 2020. Photo by Anne Wernikoff for CalMatters)
Here’s a look at California’s 10 largest cities and how they’re responding to the coronavirus fallout:
Los Angeles: Big promises in California’s biggest city
With just under a fifth of California’s confirmed cases in his city, Los Angeles Mayor Eric Garcetti has frequently acted like a governor, often steps ahead of Gov. Gavin Newsom.
Garcetti, a Democrat, halted all evictions in mid-March, weeks before California courts did the same statewide. The city has mounted 26 free testing sites, where anyone with symptoms can get tested within two days. Last week Garcetti ordered residents to cover their faces in public, a move the state has not yet taken.
When the mayor announced a philanthropic fund to send cash cards to families, particularly those with undocumented immigrant members, 56,000 immediately applied.
Despite his rising profile as “storyteller-in-chief,” Garcetti’s big plans have sometimes fallen short. He initially promised to set up 6,000 beds for homeless individuals, but it’s now more likely to be 2,000.
All these initiatives cost big money even as sales tax revenues dry up. In a recent address, Garcetti said he expected a 30% to 40% drop in the city’s hotel occupancy tax and significant decreases in sales tax revenue. Unemployment could soar to 20%.
The mayor has moved $20 million from city reserves into an emergency COVID-19 response fund, but he said the city needs help.
“There’s no question though that we’re going to have cuts,” Garcetti said. “I’m imploring our Congress, I’m imploring our president to make sure the next round (of relief) also helps bail out cities.”
San Diego: Beach town facing budget deficit
Newsom praised San Diego for taking early and bold action to house the region’s 8,000 homeless people, including procuring more than 2,000 hotel rooms as emergency isolation units. Mayor Kevin Faulconer led an effort to turn the San Diego Convention Center into a massive homeless shelter, taking in more than 800 people without stable housing.
But those extraordinary measures come with extraordinary bills for California’s second largest city. The repurposing of the convention center will cost $2.8 million per month; the hotel rooms, $6 million per month.
While federal, state and county dollars will offset some of those costs, the city’s coffers will be strained at a time when hotel tax and sales tax receipts—two key revenue streams in the tourism-centric city—are plummeting. The city faces a $250 million deficit, and Faulconer has called for cuts to libraries, recreation centers and the arts to make up the shortfall.
“Make no mistake, these are going to be some of the most significant cutbacks in San Diego history,” the Republican mayor said in late March.
San Jose: A $100 million hit to Silicon Valley
San Jose’s budget will take at least a $100 million hit because of the coronavirus pandemic, according to Mayor Sam Liccardo. And that’s still an early projection. He wouldn’t be surprised if it will be worse. “This is going to be a rough ride,” said the Democrat.
Residents have seen it before: The city endured a painful pension battle in the aftermath of the last recession, eventually losing a third of its workforce due to a hiring freeze, pay cuts and employee attrition.
Now, Silicon Valley is taking another blow as a viral hotspot. Last month, the fire department had to manage an outbreak of COVID-19 cases among its first responders. As one of the regions to be hit early, Santa Clara County was among six counties that initiated a shelter-in-place order on March 17, two days before a statewide order went into effect.
Still, the area is resilient. To help people impacted by the pandemic, the community created Silicon Valley Strong, which has raised more than $20 million to help the area’s most vulnerable residents, small businesses and nonprofits.
The current relief bill should help reimburse the city’s emergency response efforts but Liccardo hopes to see more financial help from Washington, D.C.
San Francisco: First to lockdown yet homeless remain unsheltered
San Francisco has been upheld as a model for how to deal with the pandemic but Mayor London Breed isn’t resting on her laurels. During the 1918 Spanish Flu, San Francisco introduced aggressive social distancing in the fall, tamping down the initial outbreak, only to open back up prematurely, with lethal consequences.
This year’s positive gains to date have — like all of San Francisco’s achievements — been marred by its most conspicuous failing: the city’s massive unsheltered homeless population.
So far more than 90 residents and 10 staff at San Francisco’s largest shelter have tested positive for coronavirus, the largest single cluster of cases in the city. It’s fueled criticism that the city has failed to protect its most vulnerable.
Earlier this week, San Francisco’s board of supervisors passed an ordinance demanding that Breed’s administration lease 8,250 hotel rooms, to get the estimated 8,000 people living on the street in doors by April 26. So far, the city has leased about 2,000 and sheltered nearly 800 people.
“There is no way we’re going to be able to accomplish the goals of the ordinance,” said Breed, a Democrat. Supervisors hope she rises to the challenge.
San Francisco is trying to ramp up services just as its finances are being gutted. The city’s controller recently estimated the pandemic will push the city between $1.1 and $1.7 billion into the red over the next two years — wiping out the city’s $800 million in reserves.
But those estimates are preliminary and depend on just how hard this all hits the economy — one with plenty of stay-at-home-ready tech workers, but also a disproportionate number of tourism, hospitality and restaurant workers.
“We’re in the middle of an unprecedented economic shock and we’re in the middle of a bit of data vacuum,” said Ted Egan, chief economist for the city. “There’s not a lot we do know at this point.”
Fresno: ‘Want our economy to come back’
Fresno Mayor Lee Brand first issued a shelter-in-place order for his city of more than 500,000 people on March 18, one day before the governor asked all Californians to stay at home. For the most part, the order is working, he said.
“People in Fresno get it, they’re staying at home, they want our economy to come back,” Brand said.
Prior to coronavirus, Fresno’s economy was in one of the best shapes it had been in a long time. After struggling for years to jump back from the last recession, the city’s 2020 budget boasted $34 million in reserves, the biggest in the city’s history, he said. In recent years, the city hired more police officers and boosted city services.
“We are the only city in California with a fully funded pension,” said the Republican mayor.
Last May, the city even hit a new mark: an unemployment rate under 5%. More often, Fresno’s unemployment rate is typically higher than state and national averages.
Now those gains are threatened. People are losing jobs and sales tax, a big source of city revenue, is being significantly impacted. Brand said he’d like to see cities included in another round of relief funding from the federal government.
Locally, the city set up a $750,000 fund to help small businesses. The relief program allows owners to apply for a zero-interest loan that will be forgiven after one year if their business is still operating.
Sacramento: Capital city seeks assistance
A recent influx of Bay Area transplants will help the sixth-largest city in California qualify for nearly $90 million in federal assistance from the Coronavirus Relief Fund.
Sacramento Mayor Darrell Steinberg hopes that money can buoy city coffers as California’s capital braces for a prolonged downturn. The budget for the remainder of this fiscal year, which ends June 30, should hold — but cuts loom.
“We’re going to have to figure out how to make it up,” said Steinberg spokeswoman Mary Lynne Vellinga. “We’re hoping there will be some more assistance coming down the pike.”
Sacramento will also be tested in its response to a growing population of people experiencing homelessness. Steinberg, a Democrat and co-chair of a statewide homelessness task force, has instructed staff to come up with longer-term housing strategies for people placed in temporary hotels or trailers.
Long Beach: Burning through overtime
Long Beach projects revenue losses and increased expenses brought on by the coronavirus pandemic will cost the city between $38 million and $44 million during the current fiscal year ending in September. And that’s optimistic.
City finance director John Gross noted his projections assume the city will enter a recovery period soon after May. Otherwise, he warns, the city “should be prepared for more adverse impacts.”
Long Beach is being hit by the loss of sales tax, oil revenue and a transient occupancy tax, which is paid by hotel guests. The city is also burning through staff overtime and other costs associated with its response.
The city closed down on March 19, following Los Angeles County’s “safer at home” order. So far, the majority of the city’s deaths have been linked to nursing homes and long-term care facilities.
The city has opened a free clinic at Long Beach City College, where people can be assessed and referred to testing for COVID-19. Near the clinic, the city also opened a drive-thru testing site. The centers are staffed by the city’s own Long Beach Medical Reserve Corps, a program that was in place years before the state’s recently launched Health Corps.
Oakland: Exacerbating economic and racial inequalities

On March 9, long before most mayors had to contend with the possibility of a pandemic, the Grand Princess, a ship full of contagious cruise takers, docked in the Port of Oakland.
“That’s the moment it went from being a problem in the world to a problem right here at home,” said Mayor Libby Schaaf, a Democrat.
Since then the city, like much of the Bay Area, has — so far — not seen the massive death tolls and overcrowded hospitals that were once forecast. But the pandemic has exacerbated the city’s long-standing economic and racial inequalities, said Schaaf.
Even with San Francisco across the bay, 15% of Oakland households do not have Internet access. Of the 1,100 small business owners who applied for emergency relief from a city-sponsored charity fund, seven out of 10 made less than 35% of the area’s median income.
The municipal budget has been “decimated,” Schaaf said. The city has already laid off hundreds of temporary workers.
Some of Oakland’s pre-pandemic responses to homelessness are helping. The creation of one-person shed camps and sanctioned RV parks for the homeless has reduced shelter crowding — a potential contagion cluster.
Schaaf said the city is planning to move 50 people from those group shelters into hotels. She said she hopes to convert many into permanent housing though funding is now scarce.
Bakersfield: Missed out on stimulus funding
The city of nearly 400,000 residents failed to qualify for direct federal aid under the Coronavirus Relief Fund because of the population cutoff. But Bakersfield will be able to cushion the blow thanks to a local sales tax measure passed two years ago to bolster the economy and reduce homelessness.
The tax increase has generated more than $50 million. While about half has already been allocated, money can still be tapped to help deal with the local downturn, said City Manager Christian Clegg.
“It is a saving grace,” he said. “We’ll have to be really strategic, but we’ll actually have some ability to do a few new things next year when most cities will be cutting back.”
Still, Clegg is expecting a double-digit reduction in sales tax revenue and hopes Congress will reduce the population threshold in the next round of stimulus spending.
Meanwhile, the county continues to battle the virus as the number of confirmed cases rises in Kern County. As of this week, the county reported nearly 500 COVID-19 cases with more than 300 in patients between the ages of 18 and 49.
Anaheim: An economy built on crowds
Anaheim made international headlines when Disneyland closed for the third time in history in early March, sputtering the local economy to a halt.
The pandemic has hit the city’s workforce and budget hard — both depend heavily on large groups of people bumping up against each other in the city’s theme parks, hotels and convention centers. The city believes that at least 10,000 workers in the tourism industry have lost jobs and predicts a minimum revenue loss of at least $10 million, mostly from hotel and sales tax, said city spokesman Mike Lyster.
While the city has left public health management to Orange County, it has used $1.4 million in state funds to open a third homeless shelter and has repurposed the Honda Center, usually home to the Anaheim Ducks ice hockey team, to house food bank distributions for thousands of people at a time.
Already Republican Mayor Harry Sidhu, himself the owner of several El Pollo Loco franchises, says he has a $15 million plan to restart the economy. It includes $8 million to support seniors, workers who have lost jobs and people who are struggling with rent. Nearly all of the rest would go to VisitAnaheim.org, the city’s main driver of tourism, which has laid off half of its staff. City leaders are cautiously optimistic that some restaurants could open for dine-in business again in May or June.
“The challenge for finances is getting our economy moving again as soon as it’s safe to do so,” Sidhu said. “But we know economic recovery will be gradual.”
CalMatters.org is a nonprofit, nonpartisan media venture explaining California policies and politics.
-
You Asked, We Answered: How Do I Apply for Unemployment If Under Asylum Status?
 We put the call out for your questions related to the coronavirus pandemic, and you’ve submitted questions about financial help, case counts, reopenings and more.
We put the call out for your questions related to the coronavirus pandemic, and you’ve submitted questions about financial help, case counts, reopenings and more.Listener Gigi Pravda wrote in, asking: How do I apply for unemployment benefits if under Asylum Status? How do I find financial resources in San Mateo County in the interim?
Our South Bay reporter Pamela Lorence looked into it. Here’s what she found.
(Image: Transmission electron microscopic image of an isolate from the first U.S. case of COVID-19, formerly known as 2019-nCoV. CDC / Hannah A Bullock; Azaibi Tamin)
Answer:
Unemployment for immigrants
To collect UI benefits, you must show that you were in satisfactory immigration status and authorized to work in the United States when earning the wages you used to establish your claim. You must also give proof that you are currently in satisfactory immigration status, and are authorized to work each week that you claim benefits.
Note: The EDD verifies immigration status and work authorization through the Department of Homeland Security.
You can file an unemployment insurance claim online at https://edd.ca.gov/Unemployment/UI_Online.htm.
If immigration status is questionable, this fund from private donations can help: https://www.immigrantfundca.org/
San Mateo financial resources
San Mateo County pandemic-related resources, including financial, food, health and housing resources, can be found at https://cmo.smcgov.org/covid-19-resources.
Also in San Mateo County, the Office of Community Affairs has a list of resources specifically for immigrants: https://cmo.smcgov.org/immigrant-services
Immigrants Rising in San Francisco may also be able to answer specific questions: https://immigrantsrising.org/resource/tangible-support-for-immigrant-communities-during-covid-19/
Do you have a coronavirus-related question? Submit it using the form at the right or at norcalpublicmedia.org/coronavirus. We answer questions weekly on our virtual Town Hall each Tuesday at 7 p.m. -
You Asked, We Answered: Your Questions About COVID-19 Hospitalizations, Senior Outings, and Visiting The Dentist
 We put the call out for your questions related to the coronavirus pandemic, and you’ve had plenty. We've received questions about how many people are currently hospitalized, what moving into Stage Two of reopening means for seniors, going to the dentist, and more.
We put the call out for your questions related to the coronavirus pandemic, and you’ve had plenty. We've received questions about how many people are currently hospitalized, what moving into Stage Two of reopening means for seniors, going to the dentist, and more. Here are a few answers to some of those recent submissions. We answer more each Tuesday night during our virtual coronavirus Town Hall with Sonoma County Health Officer Dr. Sundari Mase. If you have a question, please submit it using the form at the right.
How many people are currently hospitalized with COVID-19? — Vicki, Michael and Bob
You can find updated data on COVID-19 hospitalizations by county on this California Department of Public Health dashboard.
The dashboard shows the number of hospitalizations reported each day in connection with the virus. Patients are listed in four categories: hospitalized patients who have tested positive for the virus, hospitalized patients suspected of having the virus due to exhibiting symptoms typically found in COVID-19, patients in intensive care who tested positive for the virus, and patients in intensive care suspected of having the virus.
In Sonoma County as of May 20, it shows four patients in the hospital positive with COVID-19 and 24 patients suspected of having COVID-19. Two positive patients are in the ICU, and two suspected COVID-19 patients are in the ICU.
We are now entering stage 2 but what does this mean for seniors? Are they still to be going out only for essential needs? —Anonymous
People aged 65 and older are at high risk for severe illness from COVID-19. Therefore, they are strongly encouraged to stay at home as much as possible.
In Sonoma County, there is nothing in the health order that prohibits seniors from leaving home to perform allowed activities. But the order says people at high risk “should make a reasonable effort to avoid leaving home by utilizing delivery services, telecommunications, or other means available.”
"I would advise anybody who's at higher risk to still comply and remain at home," Mase said during our Tuesday Town Hall.
When will it be safe to go to the dentist for non-emergency dental work? —Anonymous
Permitted dental care in Sonoma County has recently been expanded to include more non-emergency services, including things like cleanings and other preventative care.
On May 7, the California Department of Public Health sent new guidelines to dental offices as the state moved into Stage 2 of the state's reopening plan, including criteria for dental offices to reopen. These include local infection rates, personal protective equipment requirements, and COVID-19 screenings for patients, according to the California Dental Association.
Some dentists throughout California, therefore, have started reopening for preventative care with extra precautions.
Keep an eye out at SoCoEmergency.org for additional changes to the local health order.
Do you have a coronavirus-related question? Submit it using the form at the right or at norcalpublicmedia.org/coronavirus. We answer questions weekly on our virtual Town Hall each Tuesday at 7 p.m.
-
You Asked, We Answered: Your Questions About Reopening Hair Salons, Youth Sports And How Often To Get Tested
 We put the call out for your questions related to the coronavirus pandemic, and you’ve asked about the reopening of additional business, youth sports, testing and more.
We put the call out for your questions related to the coronavirus pandemic, and you’ve asked about the reopening of additional business, youth sports, testing and more. Here are a few answers to some of those recent question submissions. We answer more each Tuesday night during our virtual coronavirus Town Hall with Sonoma County Health Officer Dr. Sundari Mase. If you have a question, please submit it using the form at the right.
Note: Our last Town Hall is scheduled for June 2. We want to know: what's the best way to get you continuing coronavirus information after that date? Let us know by using the submission form to the right and mark "Future coronavirus coverage" for question category.
When will barbershops, indoor shopping and religious services reopen in Sonoma County? —Angela, Deborah, Michelle, Barry
Even though Gov. Gavin Newsom gave approval this week for California counties who meet state requirements to begin reopening barbershops and allowing indoor shopping and religious services, those activities are still not permitted in Sonoma County.
Dr. Mase said there’s been an increase in local COVID-19 cases over the past two weeks — partly due to increased contact tracing, but also due to community transmission — that merits caution.
“I don’t think we’ve seen the full impact of what we’ve just altered with our recent shelter-in-place order, with the amendments, and so I think we’re going to wait a little bit to see where we’re going in order to protect the community,” she said.
Those recent amendments have included allowing outdoor dining at restaurants, bars and wineries, and drive-through religious services, among other changes.
Mase noted that the governor’s order applies to counties of all different sizes, with different case rates and testng capabilities.
“It’s meant for counties to look at their own situations and then make decisions as to how to move forward,” she said.
She said the county will be monitoring on a daily basis the rate of cases, the level of community transmission, the effects on vulnerable populations, PPE and hospital bed availability and other relevant data to make decisions about further reopening.
Are youth sports allowed under the recent health order amendment that allows summer day camps and other recreational programs? —David
“I think any camp is fine as long as the guidance is met,” Mase said.
The health order limits these types of programs to 12 kids or fewer per group, and the same instructor and children should be maintained in each group.
Find more details in the full health order on the county website.
How often do you recommend that members of the public get tested if we do not have symptoms? Does the recommendation change based on our job? —Anonymous
Mase said you don’t typically need to get retested after an initial COVID-19 test.
“I think people need baseline testing, and then if they become symptomatic or if they’ve had an exposure to someone with COVID, then they should be retested,” she said.
Symptoms include fever, shortness of breath, and a cough, among others. Information on how and where to get tested can be found at SoCoEmergency.org.
Watch Tuesday's Town Hall program here. Mase's interview begins at 35:45.
Do you have a coronavirus-related question? Submit it using the form at the right or at norcalpublicmedia.org/coronavirus. We answer questions weekly on our virtual Town Hall each Tuesday at 7 p.m. -
Young Artists Create Works Documenting Shelter-in-Place for Sonoma County Nonprofit
 {gallery}Art Start{/gallery}The Sonoma County arts education nonprofit Artstart has issued a call to youth artists to create and submit work that visually portrays their experience during the coronavirus pandemic.
{gallery}Art Start{/gallery}The Sonoma County arts education nonprofit Artstart has issued a call to youth artists to create and submit work that visually portrays their experience during the coronavirus pandemic.The project, called Shelter in Place: A Visual Portrayal, asks young people ages 14 to 20 to explore this moment in the world and their place in it, via drawings, paintings and sketches.
(Image: "Hope through Quarantine" By Andy Cruz, 15 / Santa Rosa, CA)
“We are at the threshold of change; this extraordinary experience offers an opportunity to reflect and express,” the project invitation reads. “Let art comfort and heal, providing a crossroads to bring people together in a new way.”
Parts of all submitted sketches will be woven into the designs for a large community mural reflecting the unique perspective of this population.
In the slideshow at the left, you can view some of the submissions that have started coming in. Artstart prompted the artists with the following questions:
- How do you currently see your role in your community?
- Where do you find hope, strength and compassion?
- What are the feelings of yourself and those around you?
- How do you see this moment in history?
To participate, send a photo of your art to
This email address is being protected from spambots. You need JavaScript enabled to view it. . Include your name, age, city and country, and tell Artstart about your piece.No special art supplies are needed, and all skill levels are welcome, from anywhere in the world.
-
Your Coronavirus Questions, Answered: Recent Protests, Access to Testing And More
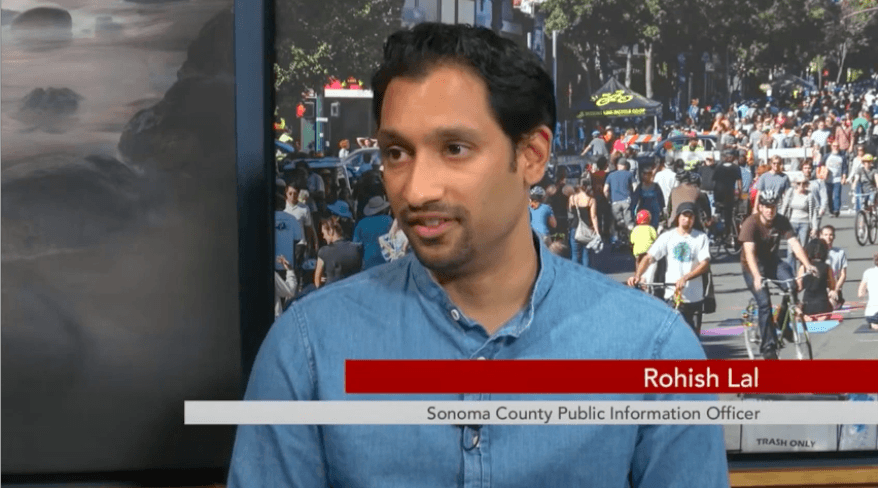
We put the call out for your questions related to the coronavirus pandemic, and you’ve asked about where you can find ongoing information, how the recent protests will affect COVID-19 case counts, access to testing and more.
Here’s what we learned from the experts during our June 2 Town Hall. Even though this was our last scheduled live Town Hall program, we will continue to cover the pandemic. Find more information below.
Last week you announced this would be the last town hall meeting. It's been very informative. Why are you stopping? Where can we get info?
Although Tuesday’s Town Hall was our last scheduled program, we will still be covering the coronavirus pandemic in our radio and TV news reports and online at NorCalPublicMedia.org. (Currently, we do daily coronavirus updates at 9:00 a.m. and 6:45 p.m. )
After 13 weeks, we felt that our weekly live TV program had run its course and we will be reassessing how we can best share information, including in smaller bites on social media.
This particular moment has reinforced the idea that the November, 2020 elections will be critical as we move collectively to choose our leaders both locally and nationally. We are going to be expending our resources to follow the issues that are important to our community, beginning with a “just recovery” from the pandemic. We’ll be paying special attention to the fact that COVID-19 cases are far more prevalent in the Latinx community than in other local groups.
Let us know how you want us to communicate ongoing coronavirus news by using the submission form to the right and marking "Future coronavirus coverage" for the question category.
Sonoma County Health Officer Dr. Sundari Mase also provides updates daily at 3:30 p.m. on Facebook live on the county’s page.
You can continue to submit questions at norcalpublicmedia.org/coronavirus, and we will keep using them to inform the direction of our reporting. When possible, we will answer them directly, and we even have hopes of involving some of you in our reporting.
How will public health trace contacts for those at a protest?
Sonoma County Public Information Officer Rohish Lal says the public health department acknowledges people’s right to protest, and if a protester does end up testing positive for COVID-19, they will conduct contact tracing as they would in any other case, to the best of their abilities.
He advises protesters to wear facial coverings, maintain physical distancing of six feet when possible, keep their hands clean and avoid touching their face.
What advice is there for testing for someone 65 and older, asymptomatic, with underlying conditions? And why are there no tests available outside the 101 corridor?
The county says that testing is a critical step in reopening which allows public health officials to identify and increase their understanding of community transmission. They want a broad sample of results from people with or without symptoms.
Dr. Mase has said you don’t typically need to get retested after an initial COVID-19 test.
“I think people need baseline testing, and then if they become symptomatic or if they’ve had an exposure to someone with COVID, then they should be retested,” she said.
If you go out to get tested, follow the same social distancing and hygiene protocols as you would at any other time.
Tests for asymptomatic members of the general public are available only in Petaluma and Santa Rosa, where most cases are concentrated. You can register to be tested here: https://lhi.care/covidtesting
By design, testing is most available in population centers in the county, but community health clinics throughout the county are taking the lead in making sure that everyone who needs a test gets one.
Watch Tuesday's Town Hall program here:
Do you have a coronavirus-related question? Submit it using the form at the right or at norcalpublicmedia.org/coronavirus.
Page 2 of 2
Northern California
Public Media
Newsletter
Get the latest updates on programs and events.

 Live Radio
Live Radio
